Airway and Ventilation Management
Video Versus Traditional Laryngoscopy for Neonatal Intubation
Last Full Review: ILCOR 2025
Endotracheal intubation in newborns is sometimes necessary for effective ventilation, particularly in the 0.4 percent to 1.2 percent of infants (Bjorland et al. 2019, e000592; Niles et al. 2017, 102) who do not respond to noninvasive methods. However, unique neonatal anatomical features, such as small airways, a large tongue and limited time to accomplish the procedure due to low lung reserves in preterm infants, make the procedure challenging. First-attempt success rates are low (46 percent) (Foglia et al. 2019, e20180902), and changes in practice, including reduced use of tracheal suction and increased reliance on noninvasive ventilation, may reduce physician proficiency.
Adverse events are common, occurring in 17 percent of cases, with 31 percent experiencing significant oxygen desaturation and reported complications, such as esophageal intubation or airway trauma (Foglia et al. 2019, e20180902). Video laryngoscopy is a technique increasingly used for emergency endotracheal intubation in adults, particularly in patients with an anticipated difficult airway, and it is more recently described for use in pediatric patients. Advantages of video laryngoscopy include improved visualization of the glottis (Brown et al. 2010, 83; Miller et al. 2023, 113), higher first-pass success rates (Miller et al. 2023, 113; Ruderman et al. 2022, 706; Warinton et al. 2024, 1373460), and the ability of a supervisor to see what the person intubating sees in real time (Antoine et al. 2024, 100776; Dias et al. 2021, e2020005009; Monette et al. 2019, 156). While video laryngoscopy has been described for intubation of neonates (Lingappan et al. 2023, CD009975), its effectiveness in the context of resuscitation at birth has not been previously reviewed systematically by ILCOR.
Red Cross Guidelines
- When resources and training are available, video laryngoscopy is suggested over traditional laryngoscopy for intubating infants at birth or in neonatal units, particularly when performed by less experienced providers. (Conditional recommendation)
- Traditional (direct) laryngoscopy remains a reasonable option as no increased harm was shown compared to video laryngoscopy.
- A traditional laryngoscope should always be available as a backup device. (Good practice statement)
Evidence Summary
An International Liaison Committee on Resuscitation (ILCOR) systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Fawke et al. 2025; Liley et al. 2025, S165) focused on the use of video laryngoscopy in infants undergoing endotracheal intubation at birth or on a neonatal unit compared with traditional laryngoscopy. Both randomized controlled trials (RCTs) (817 infants with 862 endotracheal intubations) and observational studies (3,289 infants with 3,342 intubations) met inclusion criteria for this review.
For the primary outcome of successful endotracheal intubation, there were more successful intubations with video laryngoscopy than with traditional laryngoscopy (RR, 1.43; 95% CI, 1.15–1.77), and a higher first pass successful intubation rate (RR, 1.57; 95% CI, 1.33–1.85) (Fawke et al. 2025; Liley et al. 2025, S165). For the outcome of time to successful endotracheal intubation, a benefit or harm could not be excluded. Although meta-analysis was not possible due to heterogeneity, raw data showed a slightly longer time to intubation with video laryngoscopy compared with traditional laryngoscopy in two RCTs (Geraghty et al. 2024, 1885; Moussa et al. 2016, e20152156), while two other RCTs (O’Shea et al. 2015, 912; Volz et al. 2018, 1074) found a slightly longer time to intubation with traditional laryngoscopy. A clinical benefit or harm could not be excluded for video laryngoscopy versus traditional laryngoscopy for outcomes of number of attempts to intubate, adverse events during laryngoscopy, airway trauma, bradycardia less than 100 beats per minute, bradycardia less than 60 beats per minute, oxygen saturation less than 80 percent and mortality in-hospital. Analysis of data from the included RCTs did not find a clinical benefit or harm for the outcome of esophageal intubations, but the observational studies showed possible benefit with 97 fewer esophageal intubations per 1,000 with video laryngoscopy (95% CI, 123 fewer to 22 fewer) (Fawke et al. 2025; Liley et al. 2025, S165).
There was no data to allow a subgroup analysis by location of intubation (delivery room or neonatal unit), type of intubation (emergency versus elective), gestational age, experience of the intubating person with laryngoscopy or type (design/model) of laryngoscope.
Based on the ILCOR CoSTR (Fawke et al. 2025; Liley et al. 2025, S165), a conditional recommendation was made that where resources and training allow, in infants being intubated at birth or on a neonatal unit, the use of video laryngoscopy is suggested in comparison to traditional laryngoscopy, especially in settings where less experienced staff are intubating. A weak recommendation based on very low-certainty evidence states that traditional laryngoscopy remains a reasonable option as no increased harm was shown compared to video laryngoscopy. A good practice statement states that a traditional laryngoscope should always be available as a backup device.
Insights and Implications
The ILCOR recommendation (Fawke et al. 2025; Liley et al. 2025, S165) for the use of video laryngoscopy in comparison to traditional (direct) laryngoscopy for infants being intubated at birth or on a neonatal unit was labeled as “conditional,” meaning the necessary resources and training in use of video laryngoscopy are available, particularly in settings where intubation is performed by less experienced staff. The evidence from the included RCTs that favored video laryngoscopy over traditional laryngoscopy for the outcomes of successful intubation and first pass success was graded as “high certainty” and supported by observational studies. However, video laryngoscopes are costly, require additional training and are not available in all settings. Additionally, there was no signal of increased harm shown with traditional laryngoscopy. Thus, traditional laryngoscopy remains a good alternative for neonatal endotracheal intubation.
Use of Supraglottic Airways During Chest Compressions
Last Full Review: ILCOR 2025
Positive pressure ventilation (PPV) during newborn resuscitation can be provided using a face mask, supraglottic airway (SGA) or endotracheal tube. Supraglottic airways are devices inserted into the pharynx above the glottis, allowing for effective oxygenation and ventilation. Common examples include laryngeal masks with air- or gel-filled cuffs (Mani et al. 2022, 671).
Supraglottic devices are increasingly used during neonatal resuscitation, including in newborns under 34 weeks’ gestation, as alternatives to face masks for delivering intermittent PPV. However, while they facilitate ventilation, SGAs are not considered definitive airways as are endotracheal tubes. Intubation during chest compressions is technically challenging, requiring skill and experience that may not be immediately available. A recent scoping review examines their use in newborns 34 or more weeks’ gestation receiving chest compressions despite optimized ventilation efforts.
Red Cross Guidelines
- In newborn infants 34 or more weeks’ gestation receiving chest compressions despite optimized positive pressure ventilation, if placement of an endotracheal tube is not possible or is unsuccessful, ventilation during compressions with a supraglottic airway device is reasonable. (Good practice statement)
Evidence Summary
A 2025 scoping review by the International Liaison Committee on Resuscitation (ILCOR) (Ramachandran et al. 2025; Liley et al. 2025, S165) sought evidence for the use of supraglottic airway devices, compared with face mask or tracheal tube ventilation in newborns 34 or more weeks’ gestation receiving chest compressions. Indirect evidence for the review came from newborn and adult animal studies, a neonatal manikin study, registry studies in children or adolescents and a meta-analysis of studies in adults. Results from the animal studies (Mani et al. 2022, 671; Mehrem et al. 2014, e57) suggested that compared with a tracheal tube, the use of a supraglottic airway device achieved similar rates of return of spontaneous circulation (ROSC) without compromised ventilation of the lungs. Indirect evidence from both adult and pediatric studies (Andersen et al. 2016, 1786; Forestell et al. 2024, e89; Hansen et al. 2017, 51; Le Bastard et al. 2021, 191; Wang et al. 2020, 627) suggested a reduced time-to-airway placement and increased rates of ROSC. Studies in animal models (Chen et al. 2006, 503; Liao et al. 2010, 25) suggest that epinephrine delivery by catheter down a supraglottic airway may be as effective as when delivery is via a tracheal tube. The scoping review led to a new good practice statement by ILCOR (Ramachandran et al. 2025; Liley et al. 2025, S165):
- In newborn infants 34 or more weeks’ gestation who are receiving chest compressions despite optimized positive-pressure ventilation, if placement of a tracheal tube is not possible or is unsuccessful, ventilation via a supraglottic airway device during compressions is reasonable.
Insights and Implications
Supraglottic airway devices have become popular as an alternative to face mask ventilation, as they are relatively easy to insert and are not associated with the compromised ventilation reported with face masks due to leaks around the mask or reduced tidal volume and minute volume. Of note, the ILCOR scoping review did not identify studies in newborns, and the results from indirect evidence should be interpreted with caution. Additional clinical studies are needed. Despite this, it is recognized that endotracheal tube placement is a specialized skill, and skilled personnel may not be immediately available. Supraglottic airway device placement provides an alternative when personnel skilled in newborn intubation are not available or attempts to intubate are unsuccessful. The lack of clinical data from studies with newborns means that a systematic review of the topic is not indicated, and a treatment recommendation cannot be generated from the ILCOR scoping review. In this case, the volume of indirect evidence (from animal studies and adult and pediatric studies) allows creation of the good practice statement, with the specified conditions for use of an SGA during chest compressions.
Tactile Stimulation for Resuscitation Immediately After Birth
Last Full Review: ILCOR 2022
Tactile stimulation has been recommended for decades for the initial management of infants with inadequate respiratory effort at birth. Forms of stimulation vary and may include rubbing the chest, sternum, back or soles of the feet, and flicking the soles of the feet. This intervention has never been reviewed systematically to determine its effectiveness.
Red Cross Guidelines
- For newborn infants greater than 32 week’s gestation with absent, intermittent or shallow respirations immediately after birth, it is reasonable to use tactile stimulation in addition to initial care including drying, stimulation and additional care to maintain temperature.
- Tactile stimulation should not delay the initiation of positive pressure ventilations for newborn infants who continue to have inadequate respiratory effort after birth despite initial care.
Evidence Summary
A 2022 International Liaison Committee on Resuscitation (ILCOR) systematic review (Wyckoff et al. 2022, e483) and Consensus on Science with Treatment Recommendations (CoSTR) (Wyckoff et al. 2022, e483; de Almeida et al. 2022) sought to compare the effectiveness of tactile stimulation with routine handling in newly born term and preterm infants. Eligible studies identified included two observational studies, but one was excluded from data analysis due to critical risk of bias. The remaining study (Dekker et al. 2018, 37) included 245 preterm infants on continuous positive airway pressure (CPAP) with clinical indications for tactile stimulation. Analysis of data from this study showed a reduction in tracheal intubation in infants who received tactile stimulation compared with no tactile stimulation (RR, 0.41; 95% CI, 0.20–0.85) (de Almeida et al. 2022). Anticipated absolute effects were risk with routine handling only (177 per 1,000) and risk difference with tactile stimulation in addition to routine handline, 105 fewer per 1,000 infants (95% CI, 142 fewer to 27 fewer). A weak recommendation was made by ILCOR suggesting that it is reasonable to apply tactile stimulation in addition to routine handling with measures to maintain temperature in newborn infants with absent, intermittent or shallow respirations during resuscitation immediately after birth. A good practice statement was made that tactile stimulation should not delay the initiation of positive pressure ventilation (PPV) for newborn infants who continue to have absent, intermittent or shallow respirations after birth (Wyckoff et al. 2022, e483; de Almeida et al. 2022).
In task force discussion, it was noted that the certainty of evidence from this single study is very low and results should be analyzed with caution because of indirectness (all infants were started on CPAP before tactile stimulation), possible selection bias and confounding (de Almeida et al. 2022). Observational studies not included in the review due to lack of a control group reported that infants who received tactile stimulation responded with crying, grimacing and body movements. Other studies not included in the review included a comparison of back rubbing to foot flicking, reporting no difference between both techniques in achieving crying to prevent the need for PPV. One randomized controlled trial commented on in the ILCOR CoSTR compared single versus repetitive tactile stimulation in newborn and preterm infants immediately after birth. Compared with the single tactile stimulation group, infants in the repetitive stimulation group had higher oxygen saturation levels and lower oxygen requirements at the start of transport to the neonatal intensive care unit (Wyckoff et al. 2022, e483; de Almeida et al. 2022).
Insights and Implications
The American Red Cross Scientific Advisory Council has expressed concern for the risk of intraventricular hemorrhage among preterm infants with a gestational age less than 32 weeks. The ILCOR systematic review included a single observational study (Dekker et al. 2018, 37) of 245 preterm newborn infants less than 32 weeks’ gestational age. This study showed tactile stimulation to be associated with a decreased need for tracheal intubation, but the evidence was deemed to be of very low certainty due to indirectness, possible selection bias, and confounding (retrospective analysis of tactile stimulation which could not be determined in 34 percent of the tactile stimulation episodes). No data was reported in this study for the outcome of intraventricular hemorrhage. Due to these concerns, the Red Cross guidelines limit the use of tactile stimulation to newborns at greater than 32 week’s gestational age. Further research is needed to determine if tactile stimulation at birth has clinical benefits, which patients may benefit and the efficacy of different methods of tactile stimulation. The optimal duration for applying tactile stimulation is unknown, and there are concerns that tactile stimulation may delay initiation of ventilation after birth and compromise resuscitation or that it may cause soft tissue trauma.
Suctioning Clear Amniotic Fluid at Birth
Last Full Review: ILCOR 2022
Suctioning of the mouth and nose in newborn infants has been a common practice intended to clear the upper airway of amniotic fluid and to support breathing. Evidence identified in a 2010 International Liaison Committee on Resuscitation (ILCOR) Consensus on Science with Treatment Recommendations (CoSTR) suggested that routine suctioning of healthy neonates is associated with cardiorespiratory complications (Perlman et al. 2010, S516). Routine suctioning of newborns with clear or meconium-stained amniotic fluid has not been recommended since that time. Other guidelines have recommended the use of suctioning for suspected airway obstruction or when positive pressure ventilations are needed (Wyckoff et al. 2015, S543). Is there evidence of benefit or harm from suctioning the mouth and nose of newborns?
Red Cross Guidelines
- The routine suctioning of clear amniotic fluid from the mouth and nose of newborn infants immediately after birth is not indicated.
- For suspected airway obstruction, immediate airway repositioning is indicated, and suctioning should be considered. Suctioning should be brief and begin with the mouth before the nose.
Evidence Summary
A 2022 ILCOR systematic review (Fawke et al. 2022b, 100298) and CoSTR (Fawke et al. 2022a; Wyckoff et al. 2022, e483) of newborn infants born through clear amniotic fluid sought evidence comparing the initial suctioning of the mouth and nose compared with no initial suctioning. The review identified nine randomized controlled trials and two observational studies of primarily full-term infants (Fawke et al. 2022a, 100298). Clinical benefit or harm could not be excluded in this review for the primary outcomes of receiving assisted ventilation and receiving advanced resuscitation and stabilization interventions (intubation, chest compressions and epinephrine in the delivery room). In addition, clinical benefit or harm could not be excluded for secondary outcomes of receipt and duration of oxygen supplementation, heart rate at 5 minutes, respiratory rate greater than 60 breaths per minute in the first 24 hours and multiple other secondary outcomes. The authors of the review concluded that no benefit from routine suctioning of clear amniotic fluid was found (Fawke et al. 2022a; Wyckoff et al. 2022, e483). A consistent trend of lower oxygen saturations with suctioning in the first few minutes of life was noted on graphical displays in some studies. This was supported by studies showing that the time needed to achieve target oxygen saturations was longer for infants who received suctioning at birth. A good practice statement was made that airway positioning and suctioning should be considered if airway obstruction is suspected (Fawke et al. 202ab; Wyckoff et al. 2022, e483).
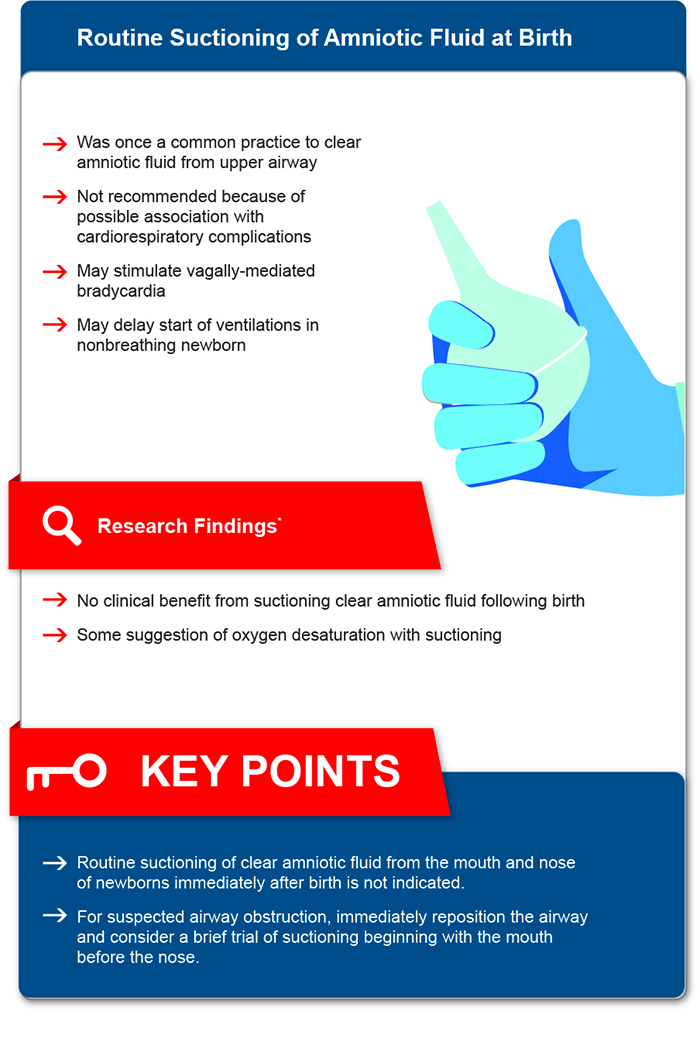
*Fawke J, Wyllie J, Udaeta E, et al. Suctioning of clear amniotic fluid at birth: A systematic review. Resusc Plus. Dec 2022;12:100298. doi:10.1016/j.resplu.2022.100298
Insights and Implications
While a benefit was not found with routine suctioning of the mouth and nose of infants born through non-meconium-stained amniotic fluid, there are concerns for potential harm. Suctioning the mouth and nose of infants born through clear, non-meconium-stained amniotic fluid has the potential to stimulate vagally mediated bradycardia and to delay the start of ventilations in nonbreathing infants. When airway obstruction is suspected, airway repositioning is indicated, and suctioning should be considered. Suctioning should be brief to avoid potential mucosal damage, prolonged hypoxia and vagally mediated bradycardia.
Exhaled Carbon Dioxide Detection to Guide Noninvasive Ventilation
Last Full Review: ILCOR 2023
Exhaled carbon dioxide (CO2) detection using a colorimetric device has been used to assess ventilation in nonintubated, bradycardic neonates, and for use in confirming correct placement of an endotracheal tube (Perlman et al. 2015, S20; Perlman et al. 2010, S516). The use of both qualitative colorimetric and quantitative side-stream capnography devices has been shown to be feasible for face mask ventilation of preterm infants in the delivery room (Hawkes et al. 2017, 74; Williams et al. 2021, 3148). Is there sufficient evidence to support guidelines for the use of exhaled CO2 monitoring to guide ventilation with noninvasive interfaces at birth?
Red Cross Guidelines
- There is insufficient evidence to suggest for the use of exhaled carbon dioxide (CO2) to guide intermittent positive-pressure ventilation with noninvasive interfaces, such as facemasks, in newborns immediately after birth.
- The routine use of colorimetric end-tidal CO2 detectors with noninvasive ventilation devices (facemasks, supraglottic airways) is not recommended during newborn resuscitation.
Evidence Summary
A 2023 International Liaison Committee on Resuscitation systematic review (Monnelly et al. 2023, 74) and Consensus on Science with Treatment Recommendations (Solevåg et al. 2023; Berg et al. 2023) sought evidence in newborn infants receiving intermittent positive pressure ventilation (IPPV) by any noninvasive interface (i.e., facemask, supraglottic airway, nasal cannulas) at birth comparing the use of exhaled CO2 monitors (i.e., waveform capnography or capnography; colorimetric devices) in addition to clinical assessment, pulse oximetry and/or electrocardiogram (ECG) with clinical assessment, pulse oximetry and/or ECG only. A prespecified primary outcome was endotracheal intubation in the delivery room with multiple resuscitation outcomes and major morbidities sought for secondary outcomes.
The literature search identified 23 papers for full test review, but no studies were identified that were designed to address the question. Eight ineligible studies that were considered useful for providing data relevant to noninvasive IPPV and CO2 monitoring immediately after birth were narratively summarized in the scoping review. The reader is encouraged to read the full summary online at https://costr.ilcor.org/document/exhaled-co2-to-guide-non-invasive-ventilation-at-birth-nls-5350-tfsr.
In short, data reported on infants receiving IPPV by facemask suggests that exhaled CO2 monitoring may help recognize airway obstruction and inadequate tidal volume delivery during IPPV (Solevåg et al. 2023; Berg et al. 2023). In addition, colorimetric CO2 detection during facemask IPPV may precede an increase in heart rate in bradycardic neonates. In other studies, the impact of real time CO2 monitoring to providers for guiding ventilatory actions could not be assessed. When an exhaled CO2 detector was used as part of a resuscitation bundle to optimize facemask IPPV in preterm infants, it was not possible to know the effectiveness of the isolated components of the bundle.
The review concludes that there is insufficient evidence to suggest for or against the use of exhaled CO2 to guide IPPV with non-invasive interfaces, such as facemasks, supraglottic airways and nasal cannulas in newborns immediately after birth (Solevåg et al. 2023; Berg et al. 2023; Monnelly et al. 2023, 74).
Insights and Implications
The studies identified in the systematic review, while encouraging, are inadequate to support a decision to use or not use capnography to guide noninvasive IPPV immediately after birth. Questions also remain about the potential risk due to undetected exhaled CO2 in newborns with absent or insufficient circulation during effective IPPV, the impact of cord management on exhaled CO2 detection, cost-effectiveness and resource requirements of exhaled CO2 monitors, and other knowledge gaps identified by the review authors (Solevåg et al. 2023; Berg et al. 2023). The Red Cross guidelines recommend against the routine use of colorimetric end-tidal CO2 detectors with noninvasive ventilation (facemasks, supraglottic airways) due to the risk of contamination with gastric contents and medications, potential distraction from other vital aspects of resuscitation and lack of evidence to support integrating use of these devices into practice.
Supraglottic Airways for Neonatal Resuscitation
Last Full Review: ILCOR 2022
Positive pressure ventilation (PPV) is used for the initial resuscitation of newborn infants and may be delivered by face mask, supraglottic airway (SGA) or endotracheal intubation. Supraglottic airways are devices inserted into the pharynx, above the glottis, for ventilation and oxygenation. These devices include laryngeal masks with either an air-filled or gel cuff (Mani et al. 2022, 733). While helping to maintain an airway for ventilation, supraglottic airway devices are not considered definitive airways. A 2015 International Liaison Committee on Resuscitation (ILCOR) review compared the use of a laryngeal mask (first generation air-filled cuff) as a primary or secondary device with face mask ventilation or endotracheal intubation (Perlman et al. 2015, S204). This review led to a weak recommendation in newborns 34 weeks’ gestation of more for a laryngeal mask to be used as an alternative to endotracheal intubation if ventilation through a face mask is unsuccessful. For the same patient population, a strong recommendation also supported the use of a laryngeal mask when endotracheal intubation is not feasible after failed PPV. Is there evidence to support the initial (primary) use of an SGA compared with a face mask for PPV in newborns during resuscitation immediately after birth?
Red Cross Guidelines
- Supraglottic airways (i.e., air-filled or gel cuff laryngeal masks) may be considered for newborn infants with a gestational age of 34 weeks or more receiving intermittent positive pressure ventilation during resuscitation immediately after birth if unable to ventilate effectively with a face mask and when healthcare professionals are present who are competent in their use.
Evidence Summary
A 2022 systematic review (Yamada et al. 2022a, e2022056568) and Consensus on Science with Treatment Recommendations (Yamada et al. 2022b) by the ILCOR focused on the use of an SGA compared with a face mask for providing PPV to newborn infants 34 0/7 weeks’ gestation or more during resuscitation immediately after birth. Five randomized controlled trials (RCTs) and one quasi-RCT (Yamada et al. 2022b; Zhu et al. 2011, 1405; Trevisanuto et al. 2015, 286; Singh 2005, 303; Pejovic et al. 2018, 255; Pejovic et al. 2020, 2138; Feroze et al. 2008, 148) with a total of 1,857 newborn infants allowed for meta-analysis of data for multiple outcomes. Of note, a strong inverse association was found between the use of an SGA compared with a face mask for the outcome of risk of endotracheal intubation (RR, 0.34; 95% CI, 0.20–0.56; P<0.001; RD, 41 fewer per 1,000 infants had endotracheal intubation during resuscitation when an SGA was used [95% CI, 49 fewer to 27 fewer]). The authors commented that this may reflect a greater likelihood of achieving effective ventilation with an SGA, but there were biases in the studies that need to be considered. An inverse relationship was found between the use of an SGA compared with a face mask for the outcome of failure to improve with device (RR, 0.24; 95% CI, 0.17–0.36; RD, 105 fewer per 1,000 infants [95% CI, 114 fewer to 88 fewer] had failure to improve when an SGA was used). The duration of PPV was found to be a mean of 62 seconds, with a mean difference of 18 seconds lower (95% CI, 24 seconds lower to 36 seconds lower) when an SGA was used. Meta-analyses could not exclude benefit or harm from use of an SGA compared with a face mask for PPV for outcomes of chest compressions during resuscitation, epinephrine administration during resuscitation, air leak during initial hospital stay, soft tissue injury and survival to hospital discharge (Wyckoff et al. 2022, e483; Yamada et al. 2022b).
Of note, data was not reported to allow subgroup analysis by gestational age (term versus late preterm). Subgroup analysis based on device design (air-filled cuff or gel cuff) showed no evidence of an interaction for the outcome of failure to improve with the device (P=0.29, I² = 10%). However, there was insufficient data to perform subgroup analysis based on device design for other outcomes (Wyckoff et al. 2022, e483; Yamada et al. 2022b).
A weak treatment recommendation by ILCOR suggests that where resources and training permit, an SGA may be used in place of a face mask for newborn infants 34 0/7 weeks’ gestation or more receiving intermittent PPV during resuscitation immediately after birth (Wyckoff et al. 202, e4832; Yamada et al. 2022b).
Insights and Implications
The Red Cross guidelines are informed by this ILCOR systematic review. The authors of the review note that an optimal information size was not achieved for any of the critical or important prespecified outcomes except for duration of PPV. In addition, while the trials included in this review used both air-filled and gel cuff laryngeal masks, there was insufficient data to perform a subgroup analysis of air-filled cuff versus gel cuff laryngeal masks except for the outcome of failure to improve with the device. A small number of adverse events were reported across all studies in this review. Additional trials are needed before stronger recommendations can be made regarding the use of SGAs as the initial device for PPV in resuscitation of newborns immediately after birth and the specific device design. It is also important to consider the potential disadvantages to the initial use of SGAs for PPV. This may include the need for training, cost requirements, cost effectiveness and potential adverse events.
Laryngoscopy and Suctioning of Meconium at Birth for Non-Vigorous Newborns
Last Full Review: ILCOR 2020
Does performing immediate laryngoscopy (with or without tracheal intubation) and suctioning at the start of resuscitation of non-vigorous infants born at 34 weeks’ or later through meconium-stained amniotic fluid, compared with performing immediate resuscitation without direct laryngoscopy at the start of resuscitation, change outcomes including survival to hospital discharge, neurodevelopmental impairment and meconium aspiration syndrome?
Red Cross Guidelines
- For non-vigorous newborns delivered with meconium-stained amniotic fluid, healthcare professionals should not routinely perform immediate laryngoscopy after birth with or without tracheal suctioning.
- For non-vigorous newborns delivered with meconium-stained amniotic fluid, healthcare professionals should perform immediate resuscitation.
- In the presence of airway obstruction, healthcare professionals may consider laryngoscopy and suctioning for newborns delivered with meconium-stained amniotic fluid and requiring resuscitation.
Evidence Summary
An International Liaison Committee on Resuscitation (ILCOR) systematic review with meta-analysis (Trevisanuto et al. 2020, 117) and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2020, S185) included four randomized controlled trials (RCTs) (Chettri, Adhisivam, and Bhat 2015, 1208; Nangia et al. 2016, 79; Singh et al. 2018, 165; Kumar, Kumar, and Basu 2019, 1825) with 581 non-vigorous newborns delivered through meconium-stained amniotic fluid. All RCTs were considered to be at high risk for bias. The pooled estimate for survival was not found to be significantly different for the immediate laryngoscopy/suctioning group compared with the immediate resuscitation without laryngoscopy group (RR, 1.01; 95% CI, 0.960–1.06; P=0.69; aRR, -0.9%; 95% CI, -3.7%–5.6%) (Trevisanuto et al. 2020, 117).
For meconium aspiration syndrome, pooled estimate from the same four RCTs showed no significant difference in the incidence of meconium aspiration syndrome between the laryngoscopy intervention group and the comparator group (RR, 1.00; 95% CI, 0.80–1.25; P=0.98; aRR, 0.0%; 95% CI, -6.9%–8.6%) (Trevisanuto et al. 2020, 117).
Other outcomes that with meta-analysis did not show a difference between laryngoscopy with suctioning and no laryngoscopy/suctioning included hypoxic-ischemic encephalopathy, use of mechanical ventilation, respiratory support excluding mechanical ventilation, chest compressions, use of epinephrine in the delivery room, endotracheal intubation for positive pressure ventilation in the delivery room, and length of hospitalization (Trevisanuto et al. 2020, 117).
A weak recommendation by ILCOR for non-vigorous newborns delivered through meconium-stained amniotic fluid suggests against routine immediate direct laryngoscopy after delivery with or without tracheal suctioning when compared with immediate resuscitation without direct laryngoscopy (Wyckoff et al. 2020, S185).
It is noted that meconium-stained amniotic fluid remains a significant risk factor for receiving advanced resuscitation in the delivery room. Rarely, an infant may require intubation and tracheal suctioning to relieve airway obstruction (Wyckoff et al. 2020, S185).
Insights and Implications
Non-vigorous infants were defined as heart rate under 100 beats per minute, decreased muscle tone and/or depressed breathing at delivery. In summary, the systematic review and meta-analysis showed that an approach based on immediate laryngoscopy with tracheal suctioning did not improve survival at discharge compared with immediate resuscitation without laryngoscopy. The ILCOR reviewers noted that in making their recommendation, they place value in both harm avoidance (i.e., delays in initiating bag-mask ventilation, potential harm of the procedure) and the unknown benefit of routine tracheal intubation and suctioning (Wyckoff et al. 2020, S185). In light of a lack of evidence for benefit from routine suctioning, they state that emphasis to be on initiating ventilation within the first minute of life for non-breathing or ineffectively breathing infants, even when born through meconium-stained amniotic fluid (Wyckoff et al. 2020, S185). A caveat is that tracheal intubation may be needed in some newborns to clear a blocked airway or for subsequent ventilation (Edwards et al. 2019; Kaira et al. 2020, 46).
Initial Oxygen Concentration for Preterm Newborn Resuscitation
Last Full Review: ILCOR 2025
Last Update: 2025
In 2019, an International Liaison Committee on Resuscitation (ILCOR) systematic review (Welsford et al. 2019, e20181828) and Consensus on Science with Treatment Recommendations (CoSTR) (Wyckoff et al. 2020, S185) concluded that in preterm newborns less than 35 weeks’ gestation who received respiratory support at birth, there was no statistically significant benefit or harm from the use of an initial lower oxygen concentration compared with a higher oxygen concentration for all-cause short-term mortality, long-term mortality, long-term neurodevelopmental impairment, retinopathy of prematurity, necrotizing enterocolitis, bronchopulmonary dysplasia and major intraventricular hemorrhage. This led to an ILCOR weak recommendation to start with a lower oxygen concentration (fraction of inspired oxygen [FiO2] 0.21 to 0.30) compared with a higher concentration (0.60 to 1.00) for preterm infants of less than 35 weeks’ gestation, with subsequent titration of oxygen based on pulse oximetry readings. The Red Cross guidelines have paralleled these recommendations. Since the 2019/2020 reviews, additional published studies evaluated the recommended oxygen concentration to use when initiating resuscitation in preterm infants, triggering an updated ILCOR systematic review.
Red Cross Guidelines
- For preterm infants born at less than 32 weeks’ gestation requiring resuscitation, it is reasonable to consider initiation of resuscitation with a fraction of inspired oxygen (FiO2) concentration of 30% or more, and titrate oxygen per pulse oximetry readings.
- For preterm infants born at 32+0 to 34+6 weeks’ gestation requiring resuscitation, consider initiating resuscitation with an FiO2 between 21% and 30% and subsequent titration of the oxygen based on pulse oximetry readings. (Good practice statement)
Evidence Summary
A 2024 individual patient data network meta-analysis (NetMotion) (Sotiropoulos et al., 2024, 774) was used by ILCOR in the adolopment process (Schünemann et al. 2017, 101). The NetMotion study analyzed data from 1,055 infants and concluded that a high initial FiO2 (0.90) may be associated with reduced mortality in preterm infants born at less than 32 weeks’ gestation compared to a low initial FiO2. An ILCOR CoSTR (International Liaison Committee on Resuscitation Neonatal Life Support Task Force, 2024; Liley et al. 2025, S165) utilized the evidence from the NetMotion individual patient data combined with study-level meta-analysis of evidence from large observational studies and eligible randomized controlled trials (RCTs) included in the 2019 systematic review (Welsford et al. 2019, e20181828) as well as evidence from additional RCTs published since 2018. The focus of the review was the use of a lower initial oxygen concentration (FiO2≤0.5) compared with a higher initial oxygen concentration (FiO2>0.5) in newborn infants less than 35 weeks’ estimated gestational age who receive respiratory support at delivery. Of note, the NetMotion individual patient data network meta-analysis (Sotiropoulos et al., 2024, 774) included 1,055 infants, all less than 32 weeks’ gestation, while the 2019 ILCOR systematic review (Welsford et al. 2019, e20181828) included infants at less than 35 weeks’ gestation. The 2025 ILCOR study-level meta-analysis included 1,289 infants.
Analysis of data from RCTs included in the individual patient network meta-analysis (Sotiropoulos et al. 2024, 774) of different initial oxygen concentrations in preterm infants showed (International Liaison Committee on Resuscitation Neonatal Life Support Task Force, 2024; Liley et al. 2025, S165):
- High initial FiO2 versus low initial FiO2: Eight RCTs involving 833 infants provided low-certainty evidence suggesting lower mortality with high initial FiO2 (aOR, 0.45; 95% CI, 0.23–0.86).
- Intermediate initial FiO2 versus low initial FiO2: Four RCTs involving 652 infants provided very low-certainty evidence showing no difference in mortality (aOR, 1.33; 95% CI, 0.54–3.15).
- High initial FiO2 versus intermediate initial FIO2: An indirect comparison of 519 infants provided very low-certainty evidence suggesting lower mortality with high initial FiO2 (aOR, 0.34; 95% CI, 0.11–0.99).
However, prediction intervals for these comparisons crossed the line of no effect, indicating inconsistency and reducing the certainty of the evidence. For other outcomes (severe intraventricular hemorrhage, chronic neonatal lung disease, retinopathy of prematurity), a benefit or harm could not be excluded when comparing high (>0.90) versus low (≤0.30) FiO2 (International Liaison Committee on Resuscitation Neonatal Life Support Task Force, 2024; Liley et al. 2025, S165).
The ILCOR study-level meta-analysis was unable to exclude a clinical benefit or harm for the comparison of a lower initial oxygen concentration (FiO2≤0.5) versus a higher initial oxygen concentration (FiO2>0.5) for multiple critical or important outcomes. No new observational studies met inclusion criteria for the 2025 CoSTR (International Liaison Committee on Resuscitation Neonatal Life Support Task Force, 2024; Liley et al. 2025, S165).
The revised 2025 ILCOR treatment recommendations (International Liaison Committee on Resuscitation Neonatal Life Support Task Force, 2024; Liley et al. 2025, S165) include a weak recommendation for newborn infants at less than 32 weeks’ gestation that it is reasonable to begin resuscitation with 30% oxygen or more. For infants born at 32 to 34+6 weeks’ gestation, there is insufficient evidence to make a recommendation.
Insights and Implications
The 2025 ILCOR CoSTR authors note that there are ongoing concerns about unmeasured adverse effects of hyperoxia and hypoxia in the study population, and two multicenter trials are underway that will compare an FiO2 of 0.30 versus 0.60 for treatment. In most of the studies included in this ILCOR review, despite the initial oxygen concentration used, oxygen saturation monitoring and individualized adjustments of the inspired oxygen concentration were used.
Past Red Cross guidelines called for using an initial oxygen concentration between 21% and 30% for resuscitation of preterm newborns less than 35+0 weeks’ gestation and to titrate oxygen concentration as needed using pulse oximetry readings. The revised guidelines now specify, based on the updated systematic review, that it is reasonable to use an initial oxygen concentration of 30% or more for preterm infants born at less than 32+0 weeks’ gestation who require resuscitation. Although the ILCOR review notes there is insufficient evidence to make a recommendation for an initial oxygen concentration for preterm infants born at 32 to 34+6 weeks’ gestation, there was no evidence of harm with lower oxygen concentrations in the previous review, and the Red Cross values the continuity of previous guideline recommendations to start with an oxygen concentration between 21% and 30% for infants born at 32+0 to 35 weeks’ gestation, followed by titration of the oxygen concentration based on pulse oximetry.
Supplemental Oxygen During Chest Compressions
Last Full Review: ILCOR 2023
A 2015 International Liaison Committee on Resuscitation (ILCOR) Consensus on Science with Treatment Recommendations (Perlman et al. 2015, S204; Wyllie et al. 2015, e169) did not identify human data to inform guidelines for the use of oxygen during cardiac compressions in newborns. A good practice statement was made to try increasing the supplementary oxygen concentration during chest compressions. The rationale for this suggestion is that by the time resuscitation of a newborn has reached the stage of providing chest compressions, steps should have been taken to attempt the return of spontaneous circulation (ROSC) using effective ventilation with low-concentration oxygen. What evidence currently supports the use of supplemental oxygen in newborn resuscitation?
Red Cross Guidelines
- Once chest compressions are initiated, the oxygen concentration should be increased to 100% and continued until the newborn’s heart rate reaches 60 or more beats per minute.
- Once compressions are no longer indicated for a newborn, the oxygen concentration should be adjusted to meet target oxygen saturation levels.
Evidence Summary
A 2023 scoping review (Ramachandran et al. 2023a, 442; Ramachandran, 2023c; Berg et al. 2023) by ILCOR sought evidence for the use of lower concentrations of oxygen versus 100% oxygen as the ventilation gas in neonates receiving cardiac compressions. No human studies were identified comparing 21% oxygen versus 100% oxygen or any other oxygen concentration during chest compression. Several animal studies were identified that compared oxygen concentrations during compression following asphyxial cardiac arrest using either 3:1 compression-to-ventilation ratio, chest compressions with asynchronous ventilations or chest compressions with sustained insufflation. No difference was reported in time-to-ROSC, mortality, lung inflammatory markers, brain inflammation or oxidative stress. No long-term outcomes were appraised.
The review concludes that the information from the studies identified was considered insufficient to alter existing ILCOR treatment recommendations (Ramachandran et al. 2023a, 442; Ramachandran, 2023c; Berg et al. 2023).
Insights and Implications
The balance between providing too little or too much oxygen is a challenge in neonatal resuscitation. Perinatal hypoxia and too little supplemental oxygen can lead to end-organ damage, while hyperoxia is associated with reduced cerebral blood flow and formation of oxygen free radicals, which factor into reperfusion injury during reoxygenation after asphyxia and multisystemic injuries. Once neonatal bradycardia has resolved and chest compressions are no longer needed, different methods can be employed for delivery of oxygen at a concentration that meets oxygen saturation target levels, thus avoiding both hypoxia and hyperoxia.
Positive Pressure Ventilations at Birth
Last Full Review: ILCOR 2021
Approximately 5 percent of term infants require respiratory support at birth with positive pressure ventilations (PPVs). Most commonly, support is provided with a flow-inflating bag, a self-inflating bag or a T-piece resuscitator. The choice of which device to use has previously been supported by bench and animal studies, but recent publications may help inform the Red Cross guidelines.
Red Cross Guidelines
- For newborns requiring positive pressure ventilation at birth, a T-piece resuscitator should be used.
- If a T-piece resuscitator is unavailable or staff are untrained/not competent in its use, a self-inflating bag, with or without a positive end-expiratory pressure valve, can be used.
Evidence Summary
The Red Cross guidelines were informed by a 2021 International Liaison Committee on Resuscitation (ILCOR) systematic review (Trevisanuto et al. 2021a) and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2021; Trevisanuto et al. 2021b) that compared the use of different devices for administering PPVs to infants at birth. Comparisons that were searched for included:
- T-piece resuscitator versus self-inflating bag.
- T-piece resuscitator versus flow-inflating bag.
- Flow-inflating bag versus self-inflating bag.
- Self-inflating bag with positive end-expiratory pressure (PEEP) versus self-inflating bag.
The primary outcome of interest was in-hospital mortality. Multiple secondary outcomes were selected. A total of six studies were ultimately included in the systematic review and meta-analysis, including five randomized controlled trials (RCTs), and one prospective cohort study that enrolled only preterm newborns. Risk of bias was judged high for the RCTs included in the completed comparisons, and moderate for the observational study. Certainty of evidence was rated as very low or low for relevant outcomes due to serious risk of bias and imprecision (Trevisanuto et al. 2021a).
For the comparison of T-piece resuscitator versus self-inflating bag, meta-analysis of data from the four RCTs (1257 infants) did not find a difference between the treatment groups for in-hospital mortality, while for the observational study, a reduction of in-hospital mortality was associated with the use of a T-piece resuscitator compared with a self-inflating bag (RR, 0.71; 95% CI, 0.63–0.80; RD, -0.13) (Trevisanuto et al. 2021a). The observational study also found that use of a T-piece resuscitator was associated with a reduced risk of intraventricular hemorrhage, severe intraventricular hemorrhage and intubation in the delivery room. A reduction in the probability of bronchopulmonary dysplasia was shown with meta-analysis for T-piece resuscitator use compared with a self-inflating bag use (RR, 0.64; 95% CI, 0.43–0.95; RD, -0.03), and a small reduction in the duration of PPV was shown with the use of a T-piece resuscitator (MD, -19.8 seconds; 95% CI, -27.7 to -12.0 seconds) (Trevisanuto et al. 2021a).
For the comparison of self-inflating bag with a PEEP valve versus a self-inflating bag without a PEEP valve, meta-analysis of two RCTs (933 infants) did not fi nd a difference between groups for the outcome of in-hospital mortality. Duration of hospital stay was slightly increased with self-inflating bag with a PEEP valve (MD, 0.14 days; 95% CI, 0.01–0.27 days) (Trevisanuto et al. 2021a). No eligible studies were identified comparing a T-piece resuscitator with a flow-inflating bag or comparing a flow-inflating bag with a self-inflating bag.
The review concludes that there is no significant difference in the risk of in-hospital mortality with T-piece resuscitator use compared with self-inflating bag use; however, resuscitation with a T-piece resuscitator compared with a self-inflating bag reduces the duration of PPV and risk of bronchopulmonary dysplasia. There is insufficient evidence to determine the effectiveness of PEEP valves when used with self-inflating bags (Trevisanuto et al. 2021a). The ILCOR treatment recommendations state that where resources permit, the use of a T-piece resuscitator is suggested over the use of a self-inflating bag (with or without a PEEP valve) in infants receiving PPV at birth (Wyckoff et al. 2021). It was noted that a self-inflating bag should be available as a backup device for the T-piece resuscitation in case of gas supply failure.
Insights and Implications
Mechanical advantages of T-piece resuscitators previously shown in bench experiments include a more precise peak inflation pressure, lower probability of unintended high-pressure inflations and the ability to apply continuous PEEP (Trevisanuto et al. 2021a). These advantages are consistent with the findings in this systematic review of a reduction of bronchopulmonary dysplasia in the T-piece resuscitator group. This may be of particular benefit in very preterm infants, although subgroup analysis by gestation was not possible in this review and future studies are needed. But, there are providers who are not familiar/competent in T-piece resuscitator use. For these individuals, it is preferable to use a self-inflating bag versus the risk for inadequate ventilation or overventilation.
While a T-piece resuscitator is a preferred method for providing respiratory support to newborns requiring PPV, many prehospital professionals and healthcare professionals who provide initial care may not have this device available. Care should not be delayed while obtaining a T-piece resuscitator. In this situation, prehospital professionals and healthcare professionals should begin respiratory support to newborns needing PPV with a self-inflating bag.
Continuous Positive Airway Pressure for Term Infant Respiratory Distress in the Delivery Room
Last Full Review: ILCOR 2022
The use of continuous positive airway pressure (CPAP) has been found to be helpful for spontaneously breathing preterm newborn infants with breathing difficulty after birth or after resuscitation and is less invasive than intubation and positive pressure ventilation (PPV). The initial use of CPAP rather than intubation and intermittent PPV is suggested by the International Liaison Committee on Resuscitation (ILCOR) for spontaneously breathing preterm newborn infants with respiratory distress requiring respiratory support in the delivery room (Wyckoff et al. 2020, S185). Since the incorporation of CPAP as a consideration into neonatal resuscitation program algorithms, an increase in pneumothorax has been reported in late preterm and term newborns who received CPAP in the delivery room, raising concerns over the safety of CPAP in this population (Classen et al. 2019, 1720). The use of CPAP for preterm and term infants with respiratory distress in the delivery room has not been reviewed systematically until recently.
Red Cross Guidelines
- There is insufficient evidence to suggest for or against the routine use of continuous positive airway pressure (CPAP) compared with no CPAP for spontaneously breathing late preterm and term newborn infants in the delivery room with respiratory distress.
Evidence Summary
A 2022 ILCOR systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Wyckoff et al. 2022, e483; Shah et al. 2022) compared the application of CPAP (with or without supplemental oxygen) to no application of CPAP (with or without supplemental oxygen) in spontaneously breathing newly born infants (34 week’s gestation or more) with respiratory distress and/or low oxygen saturations during transition after birth. Two randomized controlled trials (RCTs) (Osman et al. 2019, 597; Celebi et al. 2016, 99) with 323 newborn infants and three observational studies (Smithhart et al. 2019, e20190756; Hishikawa et al. 2015, F382) with 8,476 infants were included. Meta-analysis of the three observational studies showed a higher risk of air leak syndrome development in late preterm and term newborn infants with the use of CPAP (RR, 4.92; 95% CI, 4.13–5.87) (Shah et al. 2022). Meta-analysis of data from the two RCTs showed fewer neonatal intensive care unit (NICU) admissions, fewer infants needing NICU respiratory support and fewer deaths before hospital discharge when CPAP was used. Of note, all subjects in the two RCTs were delivered by cesarean section, and one RCT used prophylactic CPAP. There was not enough data to perform prespecified subgroup analyses, including later preterm, term and post-term infants. The certainty of evidence across all outcomes was rated as very low. The CoSTR authors determined that there was insufficient evidence to suggest for or against the routine use of CPAP compared with no CPAP for spontaneously breathing late preterm and term newborn infants in the delivery room with respiratory distress (Wyckoff et al. 2022, e483; Shah et al. 2022).
Insights and Implications
By not suggesting for or against the routine use of CPAP compared with no CPAP for spontaneously breathing late preterm and term newborn infants in the delivery room with respiratory distress, the American Red Cross Scientific Advisory Council acknowledges the potential harm identified in the observational studies with the association between CPAP use and presence of air leak syndromes. This is balanced by the potential benefit shown in reduced NICU admissions of infants born by cesarean section. Additional large RCTs are needed to assess the use of CPAP in the population of interest, and studies need to include infants delivered vaginally. As such, the Red Cross Scientific Advisory Council feels that the choice to implement CPAP should be individualized, balancing risks and benefits, and should be made by the clinician caring for the patient.
Sustained Inflation at Birth
Last Full Review: ILCOR 2020
For newborn infants who receive positive pressure ventilation (PPV) for bradycardia or ineffective respirations at birth, does initiating PPV with sustained inflation(s) greater than 1 second compared with initiating PPV with intermittent inflations lasting 1 second or less per breath change clinical outcomes?
Red Cross Guidelines
- For preterm newborn infants receiving positive pressure ventilation due to either bradycardia or ineffective respirations at birth, healthcare professionals should not use initial sustained inflation(s) greater than 5 seconds.
Evidence Summary
A 2020 International Liaison Committee on Resuscitation (ILCOR) systematic review (Foglia et al. 2021) and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2020, S185) evaluated this question, with outcomes including death before hospital discharge, death in the delivery room, death within the first 48 hours or death at latest follow-up.
For death before discharge, this review identified low-certainty evidence from nine randomized controlled trials (Linder, Högel, and Pohlandt 2005, 303; Lista et al. 2015, e457; Schwaberger 2015, e0138964; Mercadante et al. 2016, 443; Jiravisitkul, Rattanasiri, and Nuntnarumit 2017, 68; Ngan et al. 2017, F525; Abd El-Fattah et al. 2017, 409; Kirpalani et al. 2019, 1165; Hunt et al. 2019, 17), including 1,406 preterm newborns who received PPV for bradycardia or ineffective respirations at birth, not showing a significant benefit or harm from initiating PPV with sustained inflations greater than 1 second compared with PPV with intermittent inflations lasting 1 second or longer per breath (RD, 3.6%; 95% CI, -0.7%–7.9%) (Foglia et al. 2021). Similar findings were shown for the outcomes of death in the delivery room, death within the first 48 hours after birth, bronchopulmonary dysplasia, intraventricular hemorrhage grade 3 or 4, retinopathy of prematurity stage 3 or higher, use of mechanical ventilation during hospitalization and air leak during hospitalization (Wyckoff et al. 2020, S185).
Subgroup analyses by age for the outcome of death before discharge found that for newborns less than 28+0 weeks’ gestation, preterm newborns who received PPV for bradycardia or ineffective respirations at birth showed evidence of potential harm from initiating PPV with sustained inflations longer than 1 second compared with PPV with intermittent inflations lasting 1 second or longer per breath (RR, 1.38; 95% CI, 1.00–1.91; 46 more patients/1000 died before discharge with the sustained inflations [95% CI, 0 fewer to 110 more per 1000]) (Wyckoff et al. 2020, S185). For the subgroup of newborns 28+1 weeks’ to 31+6 weeks’ gestation, and the outcome of death before discharge, no significant benefit or harm was shown from initiating PPV using sustained inflations longer than 1 second compared with intermittent inflations 1 second or longer per breath (Wyckoff et al. 2020, S185). Subgroup analyses for death before discharge using sustained inflation of longer than 15 seconds duration and using sustained inflation with inspiratory pressure greater than 20 millimeters of mercury similarly found no significant benefit or harm, while a subgroup with first sustained inflation with inspiratory pressure 20 mmHg or more could not exclude benefit or harm (Wyckoff et al. 2020, S185).
A weak recommendation by ILCOR for preterm newborn infants who receive positive pressure ventilation due to bradycardia or ineffective respirations at birth suggests against the routine use of initial sustained inflation(s) greater than 5 seconds (Wyckoff et al. 2020, S185).
Due to very low confidence in the estimates of effect, it was not possible to recommend any specific duration for initial inflations for term or late preterm infants who receive positive pressure ventilations due to bradycardia or ineffective respirations at birth (Wyckoff et al. 2020, S185).
Insights and Implications
It was noted by the ILCOR reviewers that inadequate patency of the larynx in preterm infants (similar to what has been seen in preterm rabbit pups with closure of the larynx other than during a spontaneous breath) could explain the absence of benefit from sustained inflation immediately after birth (Wyckoff et al. 2020, S185). It is recognized that larger multicenter trials are needed and the total number of infants in studies so far is insufficient to have confidence in the estimate of effect. Studies were not identified comparing short duration sustained inflation (less than 5 seconds) with intermittent inflations with an inspiratory time of 1 second or longer.

