CPR Techniques and Process
Mechanical Chest Compression Devices
Last Full Review: ILCOR 2025
Last Update: 2015
Mechanical cardiopulmonary resuscitation (mCPR) devices were first developed in the 1960s, using piston-based mechanisms powered by compressed gas to deliver chest compressions. Over time, the devices have become less cumbersome, more portable and more popular in emergency medical services. There are two main types of device. Piston devices use a suction cup attached to a piston mechanism and deliver compressions by pressing directly on the sternum and actively decompressing, mimicking the natural recoil of the chest. Load-distributing band devices use a broad band that encircles the patient’s chest. The band tightens and loosens to provide compressions, distributing the force over a larger area of the thorax.
While mCPR devices offer the advantage of delivering uninterrupted and standardized compressions, their use has been restricted in most circumstances due to the inherent delay in initiating cardiopulmonary resuscitation (CPR) during the application of the device, the lack of superiority to manual CPR and evidence in past reviews suggesting some worse outcomes. Since last reviewed by the American Red Cross Scientific Advisory Council in 2022, new studies have been published and an updated systematic review has been completed by the International Liaison Committee on Resuscitation (ILCOR).
Red Cross Guidelines
- The routine use of mechanical cardiopulmonary resuscitation (mCPR) devices to replace manual compressions is not recommended in the out-of-hospital or in-hospital setting.
- Healthcare professionals may consider the use of mCPR devices in situations where sustained high-quality compressions are impractical or compromise provider safety and if the response team is skilled with usage. (Good practice statement)
- Application of mCPR devices should not delay initiation of manual chest compressions.
- When attempting to use mCPR for a person in cardiac arrest with a shockable rhythm, consider not deploying the device until after a first shock, if indicated, is delivered. (Good practice statement)
Evidence Summary
The International Liaison Committee of Resuscitation (ILCOR) updated a 2015 systematic review (Callaway et al. 2015, S84) and Consensus on Science with Treatment Recommendations (CoSTR) in 2025 (Pocock et al. 2024; Drennan et al. 2025, S72). The review evaluated survival outcomes and return of spontaneous circulation (ROSC) in adults and children with cardiac arrest in any setting who received resuscitation attempted by trained medical personnel using any type of powered automated mechanical chest compression compared with manual chest compressions. Findings from newly identified studies were combined with the trials reported in the 2015 systematic review (Callaway et al. 2015, S84) and summarized by device type and outcome.
For load-distributing band devices in the out-of-hospital setting, two studies (Gao et al. 2016, 563; Wik et al. 2014, 741) with 4364 patients did not find a benefit for favorable neurologic outcome between the group receiving mCPR and the group receiving manual CPR, while one trial (Hallstrom et al. 2006, 2620) with 767 patients found worse neurologic outcome. For survival to hospital discharge, the same three studies (Gao et al. 2016, 563; Hallstrom et al. 2006, 2620; Wik et al. 2014, 741) each reported divergent findings. For ROSC, one randomized control trial (RCT) (Wik et al. 2014, 741) found lower rates with mCPR, while a second RCT (Gao et al. 2016, 563) found higher rates of ROSC. Injury identified post-resuscitation was no different between load-distributing band mechanical and manual CPR (Koster et al. 2017, 3006; Wik et al. 2014, 741).
For piston-based devices in the out-of-hospital setting, no benefit was found from the use of the piston-based device compared with manual CPR for neurological outcome at hospital discharge, at 3 months or at 6 months (Baloglu Kaya et al. 2021, 163; Gao et al. 2016, 563); for survival at differential time points; or for ROSC (Anantharaman et al. 2017, 424; Perkins et al. 2015, 947; Rubertsson et al. 2014, 53; Smekal et al. 2011, 702). Serious injury identified post-resuscitation was no different between piston-based mechanical devices and manual CPR in one study (Koster et al. 2017, 3006).
For studies conducted in the in-hospital setting using piston-based mCPR devices, one RCT (Couper et al. 2021, 228) showed no benefit with the mCPR device for favorable neurological outcome at discharge or for survival to hospital discharge. Increased ROSC and survival to hospital discharge was found with piston-based mCPR compared with manual CPR in one trial of 150 patients (Lu et al. 2010, 496). Two other trials (202 total patients) (Baloglu Kaya et al. 2021, 163; Couper et al. 2021, 228) did not find a benefit for the outcome of ROSC with the use of mCPR compared with manual CPR.
The ILCOR treatment recommendations (Pocock et al. 2024; Drennan et al. 2025, S72) are nearly identical to 2015, but clarify the settings for cardiac arrest to include:
- A weak recommendation suggesting against the routine use of automated mechanical chest compression devices to replace manual chest compressions for out-of-hospital cardiac arrest.
- A weak recommendation suggesting against the routine use of automated mechanical chest compression devices to replace manual chest compressions for in-hospital cardiac arrest.
- A good practice statement that automated mechanical chest compression devices may be a reasonable alternative to manual chest compressions in situations where sustained high-quality manual compressions are impractical or compromise provider safety.
Insights and Implications
This review showed similar findings for critical outcomes between piston-based and load-bearing band devices, and no difference in serious injuries between mCPR devices and manual devices. A general concern with the use of mCPR devices is the inherent delay with their application and with delivering an initial shock during cardiac arrest with a shockable rhythm. The International Liaison Committee on Resuscitation notes that this concern could be alleviated by delaying application of a mechanical device until after the first shock is delivered, if indicated. This is key since each minute of delay to the first shock is associated with a significantly lower proportion of ventricular fibrillation termination and return of an organized rhythm in patients with witnessed out-of-hospital cardiac arrest (Stieglis et al. 2025, 235).
Training in the application and use of mCPR devices is important to minimize delays or pauses in compressions and to ensure proper placement. The use of mCPR devices may be appropriate in some cases of out-of-hospital cardiac arrest, such as prolonged CPR and resuscitation associated with hypothermia-induced, toxicologic-induced, and pulmonary embolism-induced cardiac arrest, and cardiac arrest with prolonged transport times. The cost of these devices is significant, ranging between $12,000 and $15,000 in the United States in 2020. This can contribute to healthcare inequity.
Head-Up CPR
Last Full Review: ILCOR 2025
Last Update: 2023
Head-up cardiopulmonary resuscitation (CPR) is an emerging strategy that involves gradual elevation of the head after CPR has been initiated, and it has been shown in studies using cadaver and porcine models to improve cerebral blood flow and cerebral perfusion pressure when combined with active compression-decompression plus impedance threshold devices. A systematic review by the International Liaison Committee on Resuscitation (ILCOR) in 2021 (Wyckoff et al. 2021, 229) included a single before-after observational study (Pepe et al. 2019, 449). This study suggested that augmented flow CPR through the addition of active compression-decompression with the use of an impedance threshold device, deferred positive pressure ventilations and gradual head and torso elevation may lead to improved short-term outcomes from cardiac arrest. However, there were limitations of the study that impacted the certainty of evidence. The International Liaison Committee on Resuscitation made a weak recommendation suggesting against the routine use of head-up CPR and suggesting that the usefulness of this approach be assessed in clinical trials or research initiatives (Wyckoff et al. 2021, 229). Since 2021, some emergency medical services systems have developed protocols for the use of a head-up CPR bundle that includes an automated head/thorax-up positioning device, a mechanical CPR device and an impedance threshold device. In addition, new studies have been published, triggering an updated systematic review.
Red Cross Guidelines
- Head-up cardiopulmonary resuscitation should not be routinely used for cardiac arrest.
Evidence Summary
The 2025 ILCOR systematic review (Main et al. 2024, 100760) and Consensus on Science with Treatment Recommendations (CoSTR) (Norii et al. 2024; Bray et al. 2025, S34) evaluated evidence for the use of head-up CPR or a head-up CPR bundle (such as head-up position, active compression/decompression, use of impedance threshold devices) for adults and children in cardiac arrest in any setting compared with standard or compression-only CPR (CO-CPR) in a supine position. Critical outcomes of interest included survival at different stages and favorable neurological status. This was an update of the initial 2021 ILCOR systematic review (Wyckoff et al. 2021, 229). Three observational studies (Pepe et al. 2019, 449; Moore et al. 2022, 9; Bachista et al. 2024, 170) met inclusion criteria, all of which were included in the original 2021 systematic review. The study by Moore (Moore et al. 2022, 9) used data from the automated controller elevation-CPR (ACE-CPR) registry, while the Bachista study (Bachista et al. 2024, 170) used data from the automated head/thorax-up positioning-CPR (AHUP-CPR) registry. In the study by Pepe et al. (Pepe et al. 2019, 449), patients received either conventional (supine) CPR or head-up/torso-up CPR, both bundled with mechanical CPR and the use of an impedance threshold device. A “pit crew” approach was taken for rapid LUCAS® Chest Compression System placement, interrupting manual compressions for no more than 5 seconds. The head-up/torso-up CPR group underwent an initial priming period of supine CPR with oxygen administration but deferred positive pressure ventilations for several minutes. Patients were then gradually placed in a reverse Trendelenburg position at approximately 20 degrees after placement of the mechanical CPR device and with simultaneous placement of an advanced airway connected to an impedance threshold device. Data showed higher rate of return of spontaneous circulation (ROSC) to hospital arrival for out-of-hospital cardiac arrest (OHCA) treated with approximately 20 degree head-up CPR compared with the group treated with supine CPR (RR, 1.90; 95% CI, 1.61–2.26; P<0.001; aRR, 16.1%; 95% CI, 20.0%–12.2%) (Pepe et al. 2019, 449).
Moore et al. (Moore et al. 2022, 9) did not find a statistically significant difference for survival to hospital discharge following OHCA between the head-up CPR bundle of care group (227 adults) and the 5,196 adult patients who received conventional CPR in a supine position. Further analysis of odds ratio of cumulative survival to hospital discharge and hospital discharge with favorable neurological function was calculated based on the time between the 9-1-1 call to the start of head-up CPR for less than 20 minutes and from 20 to 38 minutes. There was no statistically significant difference between the conventional CPR and head-up CPR groups (Moore et al. 2022, 9).
Bachista et al. (Bachista et al. 2024, 170) used data from 380 adult OHCAs who received the head-up bundle in the AHUP-CPR registry compared with 1,852 adult OHCAs with nonshockable rhythms who received conventional CPR in a supine position enrolled in two different randomized controlled trials (RCTs). Unadjusted data showed a greater likelihood of survival to hospital discharge in the head-up CPR group (7.4%, 28/380 versus 3.1%, 58/1,852). With propensity score matching, the likelihood of survival to hospital discharge increased further in the head-up CPR group (7.6%, 27/353 versus 2.8%, 10/353). For the outcome of survival with favorable neurological function, the head-up CPR bundle was associated with higher probabilities than with conventional CPR (4.2%, 15/353 versus 1.1%, 4/353; OR, 3.87; 95% CI, 1.27–11.78). However, in unadjusted analysis, rates of return of spontaneous circulation were not statistically different between the two groups (33% versus 29%) nor with adjusted analyses with propensity score matching (Bachista et al. 2024, 170).
The ILCOR treatment recommendation suggests against the use of head-up CPR or a head-up CPR bundle during CPR except in the setting of clinical trials of research initiative (Norii et al. 2024; Bray et al. 2025, S34). The review authors note the very low-certainty evidence that the head-up CPR bundle is associated with better survival and neurological outcomes. However, there are no RCTs evaluating the effect of head-up CPR or head-up CPR bundle. The studies to date have mainly evaluated a head-up CPR bundle with mechanical CPR with active compression-decompression and the use of an impedance threshold device. The optimal approach, including the angle and timing of head elevation, needs to be determined if head-up CPR proves to be beneficial.
Insights and Implications
One recent before-after observational study not included in the CoSTR evaluated end-tidal carbon dioxide (ETCO2) levels during head-up CPR or standard manual CPR on patients with OHCA, including all rhythms (Debaty et al. 2024, 110406). The study groups included 122 OHCA patients enrolled in a pre-intervention period where standard manual CPR was used and a 63-patient, post-intervention OHCA group where AHUP-CPR, active compression-decompression CPR and an impedance threshold device (ITD-16) was used. Baseline ETCO2 values were comparable between the two groups, but during CPR, the head-up CPR group’s ETCO2 values were significantly higher than the conventional CPR group (40.7 millimeters of mercury (mmHg) versus 30.3 mmHg) and approached physiologic levels, regardless of the presenting rhythm. However, all clinical survival outcomes did not differ between the two groups (Debaty et al. 2024, 110406).
The ILCOR review makes important points about the lack of any RCTs and the lack of studies to determine an optimal angle and timing of head elevation. In addition, the equipment to provide a head-up CPR bundle and the necessary training is expensive and requires additional resources. Transitioning a person in cardiac arrest from supine to a head-up position is logistically challenging and may create interruptions in delivery of compressions. If manual compressions are used in a head-up position, they may be less effective than mechanical CPR devices or compressions delivered to a person in the supine position. Head-up CPR is promising but requires further research.
Rhythm Analysis During Chest Compressions
Last Full Review: ILCOR 2020
Last Update: 2021
Interrupting chest compressions during cardiopulmonary resuscitation (CPR) to check for the presence of a rhythm, or to determine if a rhythm has become shockable, can contribute to a reduced chest compression fraction (CCF), leading to decreased coronary and cerebral blood flow, which reduces the potential for survival.
Red Cross Guidelines
- Immediately after a shock is delivered, cardiopulmonary resuscitation (CPR) should be resumed for 2 minutes before pausing compressions to check for or analyze a rhythm.
- Based on the clinical situation, performing rhythm analysis after defibrillation may be considered by healthcare professionals.
- Compressions should be paused for rhythm analysis, even when using devices with artifact-filtering algorithms.
- After every 2 minutes of CPR, the rhythm should be reassessed (while minimizing interruptions to CPR for no more than 10 seconds).
- If there are physiologic signs of return of spontaneous circulation, briefly pausing compressions for rhythm analysis may be considered.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council literature update identified a single observational study enrolling 3,601 out-of-hospital cardiac arrests (Hanisch et al. 2020, e015599). This study analyzed the frequency of interruptions greater than 1 second in chest compressions, the reasons for and the duration of interruption, and how they changed between 2007 and 2016. Most compression interruptions were associated with cardiac rhythm analysis. Manual electrocardiogram rhythm analysis and pulse checks accounted for 41.6 percent of total interruption time, with a median individual interruption time of 8 seconds. Automated external defibrillator rhythm analysis accounted for 13.7 percent of total interruption time (median 17 seconds) and manual rhythm analysis and shock delivery accounted for 8.0 percent of total interruption time (median 9 seconds).
While this study does not evaluate outcomes from chest compression interruptions, it demonstrates the extent of the interruption produced from rhythm analysis, both manual and with automated external defibrillator analysis, supporting the Red Cross guidelines to immediately resume chest compressions following defibrillation. Reducing chest compression interruption time remains paramount to improved CCF and improved outcomes. This topic was last reviewed systematically by the International Liaison Committee on Resuscitation (ILCOR) in 2020 with findings suggesting potential harm associated with an immediate check for cardiac rhythm following defibrillation. A previous ILCOR review (Travers et al. 2015, S51) recommended against the routine use of artifact-filtering algorithms for analysis of electrocardiographic rhythm during CPR and recommended that their usefulness be assessed in clinical trials or research initiatives.
Insights and Implications
There may be unique situations where a rhythm analysis is warranted. As such, healthcare professionals may, in these cases, consider a rhythm analysis but should minimize the duration of the interruption in compressions.
CPR and Defibrillation in the Prone Patient
Last Full Review: American Red Cross Scientific Advisory Council 2022; ILCOR 2021
The coronavirus disease 2019 (COVID-19) pandemic has led to the further use of the prone position to improve oxygenation, with and without advanced airway management. This has led to questions regarding the feasibility of performing cardiopulmonary resuscitation (CPR) and defibrillation with the patient in the prone position and its effectiveness compared with resuscitation in the supine position.
Red Cross Guidelines
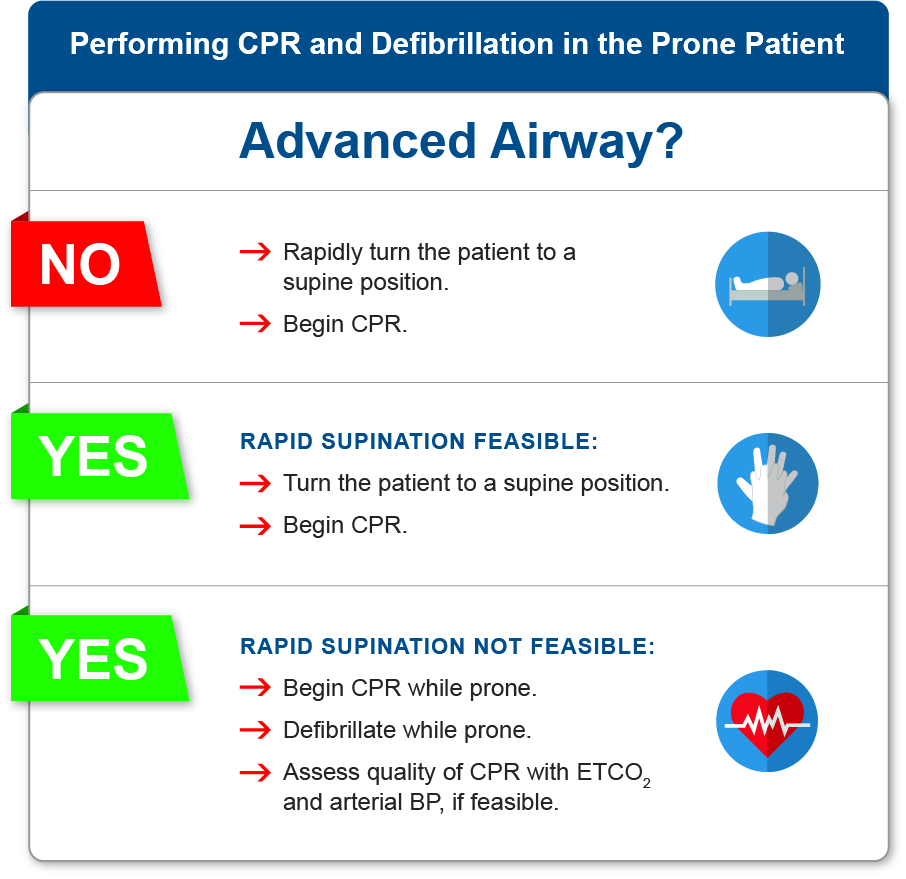
For patients in a prone position who develop cardiac arrest:
- If an advanced airway is not in place, the patient should be turned to a supine position as quickly as possible, and cardiopulmonary resuscitation (CPR) initiated.
- If an advanced airway is in place and immediate supination is not feasible or poses a risk to the patient, CPR should begin while the patient is prone.
- If the patient cannot be immediately supinated, defibrillation should be attempted in the prone position.
- For patients with an advanced airway in place in the prone position while receiving CPR, the quality of CPR should be assessed with end-tidal carbon dioxide and arterial blood pressure monitoring, if feasible.
Evidence Summary
A 2021 systematic review (Berg et al. 2021) and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2021; Wyckoff et al. 2022, e645) by the International Liaison Committee on Resuscitation (ILCOR) focused on CPR and defibrillation for cardiac arrest in adults and children in any setting when in the prone position, compared with turning the patient to the supine position prior to the initiation of CPR and/or defibrillation. Outcomes of interest included survival with/without favorable neurologic outcome, return of spontaneous circulation, end-tidal carbon dioxide (ETCO2) and arterial blood pressure readings during CPR, and time to defibrillation.
The search included all years. Two prospective nonrandomized studies and two simulation studies were identified. An additional 20 adult case reports were included, of which 12 had CPR initiated while in a prone position, and the remaining cases were supinated before starting CPR. The operating room was the predominant setting for case reports (Berg et al. 2021).
The majority of evidence included for this review was assessed to be of very low certainty and difficult to interpret. The authors of the review commented that each case may be unique and require weighing the potential risk of delayed CPR and defibrillation against the possible risk of less effective CPR and defibrillation while prone. It was noted that it may be difficult to supinate a patient who is prone and mechanically ventilated and with capnography and additional arterial lines in place. In addition, the etiology of the cardiac arrest may define the urgency of supination (Berg et al. 2021).
The treatment recommendations stemming from this review include several good practice statements, reflecting the lack of higher certainty evidence. A strong recommendation was made, for patients with cardiac arrest occurring while in the prone position without an advanced airway already in place, to turn that patient to the supine position as quickly as possible and begin CPR (Berg et al. 2021). For patients with cardiac arrest while in the prone position with an advanced airway already in place, and where immediate supination is not feasible or poses a significant risk to the patient, initiating CPR while the patient is still prone may be a reasonable approach (good practice statement). Invasive blood pressure monitoring and continuous ETCO2 monitoring may be useful to ascertain whether or not prone compressions are meeting benchmarks for adequate perfusion, and this information could inform decision-making on when to prioritize supination (good practice statement). For patients with cardiac arrest with a shockable rhythm who are in the prone position and cannot be supinated immediately, attempting defibrillation in the prone position is a reasonable approach (good practice statement) (Berg et al. 2021).
Insights and Implications
Use of the prone position in the critical care of COVID-19 patients became commonplace over a short time, and the lack of comparative outcomes data makes it difficult to inform treatment recommendations. The ILCOR recommendations stem from a review of the best available evidence combined with task force discussion and expert consensus to create good practice statements that are reflected in the new Red Cross guidelines. Further research will be needed to address knowledge gaps, such as the time needed to supinate a patient with advanced airway in place, optimal hand and defibrillator pad placement while prone, and clinical outcomes following CPR or defibrillation while in the prone position.
Extracorporeal CPR for Cardiac Arrest
Last Full Review: ILCOR 2023
Last Update: 2024
Extracorporeal cardiopulmonary resuscitation (ECPR) involves the use of extracorporeal membrane oxygenation (ECMO) to provide perfusion to end-organs during cardiac arrest when conventional resuscitation methods fail. Extracorporeal cardiopulmonary resuscitation can serve as a bridge to more definitive treatments, such as coronary angioplasty, while providing additional time to identify reversible causes of cardiac arrest.
Red Cross Guidelines
- Extracorporeal cardiopulmonary resuscitation, or cardiopulmonary resuscitation with extracorporeal membrane oxygenation, may be considered as a rescue therapy on a case-by-case basis for selected adult populations with cardiac arrest refractory to conventional resuscitation and in settings where capability and defined protocols exist.
Evidence Summary
A systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (International Liaison Committee on Resuscitation 2023; Greif et al. 2024), updated in 2024 by the International Liaison Committee on Resuscitation (ILCOR) (International Liaison Committee on Resuscitation 2024) sought evidence for the use of ECPR, including ECMO or cardiopulmonary bypass, in adults with cardiac arrest in the out-of-hospital or in-hospital setting, compared with manual or mechanical cardiopulmonary resuscitation (CPR). The review was an update of a 2023 systematic review (Holmberg et al, 2023, 109665) by ILCOR on the same topic, performed after new evidence became available. The update identified one randomized controlled trial (RCT) that was added to three RCTs evaluated in the previous reviews (Holmberg et al. 2023, 109665; Holmberg et al. 2018, 91).
The observational studies included in the previous systematic reviews were limited by a critical risk of bias. For this reason, the 2024 updated systematic review was limited to RCTs. Meta-analyses were not performed due to heterogeneity between the RCTs, and findings were reported narratively as follows (International Liaison Committee on Resuscitation 2024; Greif et al. 2024, e580):
- An RCT by Yannopoulos et al. (Yannopoulos 2020, 1807) included 30 adults with out-of-hospital cardiac arrest (OHCA). For patients receiving ECPR compared with standard care, beneficial outcomes included:
- Improved survival to hospital discharge (ARD, 36%; 95% CI, 7.4%–65%)
- Survival to 6 months (ARC 43%; 95% CI, 17%–69%)
- Favorable neurological outcome at hospital discharge (ARD, 21%, 95% CI, 0%–43%)
- Favorable neurological outcome at 6 months (ARD, 43%; 95% CI, 17%–69%)
- An RCT by Hsu et al. (Hsu et al. 2021, 92) included 15 adult OHCAs and was terminated early due to low enrollment. The trial failed to show a benefit from an ECPR strategy compared with standard care for survival to hospital discharge, survival to 3 months and favorable neurological outcome at hospital discharge and at 3 months.
- An RCT by Belohlavek et al. (Belohlavek et al. 2022, 737) included 264 adults with OHCA. A benefit was not shown from an ECPR strategy compared with standard care for survival to 30 or 180 days or for favorable neurological outcome at 180 days. However, a benefit was seen with ECPR for favorable neurological outcome at 30 days (ARD, 13%; 95% CI, 2.0%-23%).
- In the most recent RCT, Suverein et al. (Suverein et al. 2023, 299) included 134 adults with OHCA. No benefit was shown from an ECPR strategy compared with standard care for survival to hospital discharge, and for favorable neurological outcome at 30 days or 6 months.
The evidence from the four RCTs was considered low certainty. Studies included highly selected patients for ECPR, rather than the general population of all cardiac arrest cases. Some trials included patients with an initial shockable rhythm, some with any initial rhythm, and the timing of randomization varied. Thus, the CoSTR authors note that findings from the individual trials should be interpreted with caution (International Liaison Committee on Resuscitation 2024; Greif et al. 2024). Despite these concerns, the authors note that the balance of evidence suggests that for some patients with refractory cardiac arrest, ECPR may be beneficial. No direct evidence was found for ECPR with in-hospital cardiac arrest (IHCA), but trials that have suggested benefit from ECPR focused on patients with an initial shockable rhythm.
A weak recommendation by ILCOR suggests that ECPR may be considered as a rescue therapy for selected adults with OHCA when conventional CPR is failing to restore spontaneous circulation, in settings where this can be implemented. A similar weak recommendation based on very-low certainty evidence was made that ECPR may be considered as a rescue therapy for selected adults with IHCA when conventional CPR is failing to restore spontaneous circulation, in settings where this can be implemented (International Liaison Committee on Resuscitation 2024; Greif et al. 2024, e580).
Insights and Implications
While ECPR holds promise for improving survival from cardiac arrest, there are significant obstacles to its widespread use. The process is expensive, resource intensive, and not available in most OHCA settings and many hospital settings. There are ethical considerations when selecting patients, such as potential risks versus benefits, patient prognosis and quality of life. Extracorporeal cardiopulmonary resuscitation programs require significant coordination and specialized infrastructure to implement effectively. Additional research is needed to determine which patients will benefit most from ECPR, the timing and the method for providing ECPR.
CPR-Induced Consciousness
Last Full Review: ILCOR 2021; American Red Cross Scientific Advisory Council 2023
Last Update: 2024
Consciousness of a person in cardiac arrest during CPR is occasionally described by rescuers. Some survivors of cardiac arrest also describe awareness during CPR, or describe near-death experiences with some degree of recall of the resuscitation event. Is any intervention indicated when consciousness is observed during CPR?
Red Cross Guidelines
- Sedatives and/or analgesics used in critical care may be considered in small doses for patients with possible consciousness during CPR. (Good practice statement)
Evidence Summary
A 2021 scoping review (Wyckoff et al. 2021, 229; Wyckoff et al. 2022, e645; West et al. 2021) by ILCOR sought to identify published and unpublished studies, case reports and series, and grey literature related to the use of sedation, analgesia or another intervention to prevent consciousness in adults in any setting during CPR. Outcomes of interest included any clinical outcome, arrest outcomes and psychological well-being post-arrest. The review sought to describe specific cardiac arrest experiences and any interventions, such as the use of sedatives to prevent those experiences while assessing the need for a future systematic review. Five observational studies were identified evaluating different aspects of sedation and consciousness, as well as case reports with a total of 31 patients.
A narrative summary of the evidence noted several important points (West et al. 2021). First, based on two of the included observational studies (Olaussen et al. 2016, 186; Doan et al. 2020, 769) including 39,569 patients, the estimated true prevalence rate of CPR-induced consciousness is very low, between 0.23 percent and 0.7 percent. Increased rates of return of spontaneous circulation (ROSC) and survival to hospital admission and to discharge were noted in those with CPR-induced consciousness compared with patients without signs of CPR-induced consciousness. Sedation was rarely used in CPR-induced consciousness, and rescuer distress was found to be a common outcome. Pharmacological intervention rates ranged between studies from 11.5 percent to 39.7 percent for CPR-interfering consciousness. Dosing of sedatives or analgesics during resuscitation is unclear, and their use may negatively impact survival outcomes.
The ILCOR Advanced Life Support Task Force discussed the findings of this scoping review and made the following good practice statements: (Wyckoff et al. 2021; Wyckoff et al. 2022, e645)
- In settings where it is feasible, rescuers may consider using sedative or analgesic drugs (or both) in very small doses to prevent pain and distress to patients who are conscious during CPR.
- Neuromuscular-blocking drugs alone should not be given to conscious patients.
- The optimal drug regimen for sedation and analgesia during CPR is uncertain. Regimens can be based on those used in critically ill patients and according to local protocols.
Insights and Implications
Cardiac arrest experiences relayed by survivors are described differently and may include near-death experiences, out-of-body experiences, visual or auditory awareness, spiritual experiences or consciousness during CPR. Sedatives and analgesics have potential hemodynamic effects that may contribute negatively to survival outcomes and may potentially mask clinical signs of ROSC. These potential risks must be weighed against their benefit. The good practice statements by ILCOR provide reasonable suggestions for preventing pain and distress in patients who are conscious during CPR, but with the caveat of using local protocols and regimens in place for critical care patients.