CPR Techniques and Process
Continuous Chest Compression CPR Versus Standard CPR for EMS
Last Full Review: ILCOR 2025
Last Update: 2021
Many emergency medical services (EMS) systems now use a minimally interrupted cardiac resuscitation strategy as part of a bundle of care as an alternative to conventional cardiopulmonary resuscitation (CPR) with a compression-to-ventilation ratio of 30:2 for witnessed out-of-hospital cardiac arrest (OHCA). A 2017 International Liaison Committee on Resuscitation (ILCOR) review (Olasveengen et al. 2017, e424; Ashoor et al. 2017, 112) evaluated evidence for continuous chest compression CPR for OHCA combined with positive pressure ventilations using bag-mask ventilation at 10 breaths per minute, an endotracheal tube, a supraglottic airway, and by passive oxygenation through an oropharyngeal airway and an oxygen mask. Although an increase in survival was reported with the minimally interrupted chest compression approach, improvement in favorable neurologic function rates were not associated with a minimally interrupted chest compression approach compared with conventional CPR. This review was updated for 2025.
Red Cross Guidelines
For emergency medical services professionals:
- Standard cardiopulmonary resuscitation with a compression-to-ventilation ratio of 30:2 should be used for adults in cardiac arrest without an advanced airway,
OR
- Continuous chest compressions should be provided with positive pressure (bag-valve-mask) ventilations delivered without pausing chest compressions until a tracheal tube or supraglottic device has been placed.
- With an advanced airway in place, healthcare and prehospital professionals should not pause compressions for positive pressure ventilation.
Evidence Summary
A 2025 ILCOR systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Nehme et al. 2024; Bray et al. 2025, S34) evaluated evidence for the use of continuous chest compressions delivered by EMS with or without ventilations compared with standard CPR at any compression-to-ventilation ratio. The four studies meeting inclusion criteria were a large cluster randomized controlled trial (RCT) with crossover (Nichol et al. 2015, 2203) and three cohort studies (Bobrow et al. 2008, 1158; Schmicker et al. 2021, 31; Grunau et al. 2018, e3386). The cluster RCT (Nichol et al. 2015, 2203) randomized OHCA patients to receive either continuous chest compressions with asynchronous positive pressure ventilations or standard CPR (CV-CPR) with a compression-to-ventilation ratio of 30:2. A significant difference was not shown for favorable neurological survival at discharge, survival to hospital discharge, or return of spontaneous circulation with continuous chest compressions compared with conventional CV-CPR.
A cohort study (Schmicker et al. 2021, 31) of OHCA patients showed improved survival to hospital discharge with continuous chest compressions compared to standard CV-CPR, but there was poor adherence to the randomization strategy. In further analysis of cases where the randomized strategy was adhered to, continuous chest compressions had significantly lower survival rates, and patients in the 30:2 compression-to-ventilation strategy had higher survival. A 2008 cohort study (Bobrow et al. 2008, 1158) included in the 2017 ILCOR systematic review found that a minimally interrupted cardiac resuscitation protocol was associated with improved survival to hospital discharge compared with conventional 15:2 compression-to-ventilation CPR, stacked shocks, and post-shock rhythm checks (Nehme et al. 2024; Bray et al. 2025, S34).
A strong treatment recommendation was made by ILCOR that EMS providers perform CPR with 30 compressions to 2 ventilations OR continuous chest compressions with positive pressure ventilation delivered without pausing chest compressions until a tracheal tube or supraglottic device has been placed (Nehme et al. 2024; Bray et al. 2025,S34).
A recommendation from 2017 that supported systems with minimally interrupted cardiac resuscitation for witnessed shockable OHCA was removed, as the single study reporting on this intervention has a serious risk of bias from uncontrolled confounding, and the continuous chest compressions implemented were part of a bundle of practices, making it unclear if the treatment effect was related to the continuous chest compressions or other introduced practices (Nehme et al. 2024a; Bray et al. 2025, S34).
Insights and Implications
The ILCOR review noted that there is no high-quality evidence to support the superiority of either continuous chest compressions or standard CV-CPR for patient outcomes in OHCA. Pauses for delivery of ventilations produce an interruption in chest compressions, which may impact coronary and aortic blood flow (Berg et al. 2001, 2465). By providing continuous chest compressions with asynchronous positive pressure ventilations, chest compression quality may not be compromised while providing adequate oxygenation. The Red Cross guidelines have been updated based on this review and now include the choice of standard compression-ventilation CPR or the use of continuous chest compressions with positive pressure ventilations delivered without pausing chest compressions until a tracheal tube or supraglottic device has been placed.
Continuous Chest Compression CPR Versus Standard CPR for In-Hospital Cardiac Arrest
Last Full Review: ILCOR 2025
Last Update: 2017
Most research into resuscitation from cardiac arrest comes from the out-of-hospital setting, with findings contributing indirect evidence to cardiac arrest occurring in the in-hospital setting. In-hospital cardiac arrest (IHCA) is estimated to account for about 300,000 events each year in the United States (Holmberg et al. 2019, e005580). In 2023 the International Liaison Committee on Resuscitation (ILCOR) launched an initiative to provide strategic guidance to improve IHCA care using 10 steps (Chan et al. 2023, 109996). Delivering guideline-based resuscitative care is one key step toward improving IHCA quality of care and outcomes. An updated systematic review by ILCOR took a fresh look at the provision of cardiopulmonary resuscitation (CPR) to patients with IHCA.
Red Cross Guidelines
For in-hospital healthcare professionals caring for adults in cardiac arrest (Good practice statements):
- Standard cardiopulmonary resuscitation should be provided with 30 compressions to 2 ventilations,
OR
- Continuous chest compressions should be provided with positive pressure ventilations delivered without pausing chest compressions with or without an advanced airway in place.
Evidence Summary
A 2025 ILCOR systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Bray et al. 2024; Bray et al. 2025, S34) sought evidence for the provision of continuous chest compressions with or without ventilations by in-hospital providers to adults and children with cardiac arrest in any setting, compared with standard CPR (defined as any compression-to-ventilation ratio) delivered by in-hospital providers. This was an update of a 2017 ILCOR systematic review (Ashoor et al. 2017, 112) with a revised search strategy and a review plan that excluded observational studies not reporting adjusted outcomes (due to imbalances between groups known to influence survival). Studies using automated CPR or mechanical devices were only included if administered to all treatment arms. One study from the 2017 systematic review (Ashoor et al. 2017, 112) in the updated review included a cohort study that evaluated the effect of continuous chest compressions with a piston-based mechanical compression device in patients admitted to an emergency department after out-of-hospital cardiac arrest (OHCA) (Lee et al. 2013, 158). Evidence from this study was rated as very low certainty due to risk of bias and very serious imprecision. In adjusted analysis, the study showed increased survival to hospital discharge and return of spontaneous circulation (ROSC) in patients who received mechanical chest compressions and tracheal intubation with positive pressure ventilations without pausing chest compressions when compared to patients who received mechanical chest compressions interrupted for ventilation at a ratio of 5 compressions to 1 ventilation (Bray et al. 2024; Bray et al. 2025, S34).
The lack of direct evidence for this question led to a good practice statement by ILCOR:
- In-hospital providers should perform CPR with 30 compressions to 2 ventilations or continuous chest compressions with positive pressure ventilations delivered without pausing chest compressions in adults in cardiac arrest (Bray et al. 2024; Bray et al. 2025, S34).
Insights and Implications
The ILCOR review (Bray et al. 2024; Bray et al. 2025 S24) noted that interruptions in chest compressions have been associated with poorer clinical outcomes in observational studies (Christenson et al. 2009, 1241) and pauses for ventilations produce interruptions in chest compressions that may negatively impact coronary and aortic blood flow (Berg et al. 2001, 2465). A similar review for emergency medical services (EMS) identified a large high-quality randomized controlled trial that did not find a difference in patient outcomes with ventilations at a rate of 10 per minute without pausing compressions compared with a 30 compressions to 2 ventilations ratio before intubation (Nichol et al. 2015, 2203). The good practice statement is consistent with that for EMS providers.
Real-Time Feedback Devices for Ventilation Quality
Last Full Review: ILCOR 2025
Feedback devices for performing or training in the delivery of chest compressions have become common and include integrated manikin feedback systems, wearable and standalone feedback devices, and app-based feedback systems. Real-time feedback systems have recently been developed to help improve ventilation in real time during cardiopulmonary resuscitation (CPR) in out-of-hospital cardiac arrest (OHCA) scenarios. These devices have not been included in other reviews of CPR feedback devices, although there have been studies (Benoit et al. 2023, 109662; Vissers et al. 2019, 243) suggesting that ventilation during resuscitation may not meet guideline recommendations.
Red Cross Guidelines
- No recommendation. Ventilation feedback devices are an emerging technology that require further clinical studies.
Evidence Summary
A 2025 International Liaison Committee on Resuscitation (ILCOR) scoping review (Debaty et al. 2025; Bray et al. 2025, S34) sought evidence from the adult and pediatric literature and grey literature on the use of real-time ventilation quality feedback (e.g., tidal volume, adequate ventilation, mask leak, ventilation rate) in cardiac arrest.
The review identified one randomized controlled trial (RCT), two before-after prospective studies, two observational studies and 13 simulation studies. Clinical outcomes including survival to discharge, survival with good neurological outcome and return of spontaneous circulation (ROSC) were assessed in the RCT, although no data was provided on ventilation quality. One prospective observational study (Abella et al. 2007, 54) evaluated survival to discharge and ROSC following introduction of a feedback device assessing ventilation rate by thoracic impedance. A second prospective study (Drennan et al. 2024, 110381) evaluated the association between ROSC and ventilation rate and insufflation volume using a visual real-time feedback device with a pressure-flow sensor. Neither of these studies found a change in patient outcomes, but improved ventilation parameters were observed with the feedback devices. The simulation studies primarily assessed visual feedback devices for insufflation volume and ventilation rate during CPR. Most of the studies reported improvements in ventilation quality with feedback device use. Three manikin studies (Heo et al. 2020, 278; Lemaine et al. 2024, S215; Wagner et al. 2022, 1762) included pediatric scenarios and assessment of insufflation volume during bag mask ventilation. The review concludes that the current evidence is insufficient to demonstrate the clinical efficacy or effectiveness of real-time ventilation feedback devices. No good practice statements were made by ILCOR for this scoping review (Debaty et al. 2025; Bray et al. 2025, S34).
Insights and Implications
Over a third of the studies identified were sponsored by or performed by industry, and definitions of ventilation parameters assessed by the devices were not standardized. While promising technology, further non-industry-sponsored clinical studies are needed in adults and children.
Pulse Check Accuracy in Infants and Children During Resuscitation
Last Full Review: ILCOR 2025
Assessment of a child or infant begins with checking for responsiveness and obvious life-threatening bleeding. For an unresponsive child or infant, the A-B-C (airway-breathing-circulation) mnemonic is traditionally used to guide assessment, beginning with opening the Airway, and checking for the presence or absence of normal Breathing. If the child or infant is unresponsive and not breathing normally, they are considered to be in cardiac arrest and CPR is initiated. Past recommendations for healthcare professionals have included a check for Circulation with a carotid pulse in children or a brachial pulse in infants for no more than 10 seconds. However, pulses can be difficult to palpate, even for experienced healthcare professionals, and new methods of assessing circulation have developed, including ultrasound, end-tidal carbon dioxide (ETCO2) levels and pulse oximetry. This topic was prioritized for review by the International Liaison Committee on Resuscitation (ILCOR) in 2024.
Red Cross Guidelines
- In unresponsive children and infants with no signs of life and with abnormal or no breathing, lay providers and healthcare professionals should not delay cardiopulmonary resuscitation (CPR) to perform a pulse check.
- In a child or infant with no signs of life (unconscious/unresponsive) and with abnormal or no breathing, healthcare professionals may consider checking for a carotid pulse (children) or a brachial pulse (infants) in situations where alternative means are simultaneously in place for detecting a pulse or adequate perfusion. Determination of a pulse and adequate perfusion using a pulse plus a secondary method (e.g., end-tidal carbon dioxide levels, ultrasound) should take no more than 10 seconds and if absent, CPR should be initiated. (Good practice statement)
Evidence Summary
In 2024, ILCOR conducted a systematic review and developed a Consensus on Science with Treatment Recommendations (CoSTR) (Katzenschlager et al. 2024; Scholefield et al. 2025, S116) to evaluate the effectiveness of various pulse assessment sites and methods in infants and children suspected of cardiac arrest. The review (Katzenschlager et al. 2024) aimed to determine whether alternative pulse check locations (such as the femoral artery) or techniques (including cardiac auscultation, pulse oximetry, ultrasonography, monitoring ETCO2 levels and invasive monitoring) offer advantages over the traditional guideline-recommended sites (brachial pulse for infants and carotid pulse for children and adolescents) in deciding when to initiate or continue cardiopulmonary resuscitation (CPR). Outcomes of interest for this review were accuracy (sensitivity and specificity of detecting a perfusing rhythm), duration of cardiac compression pauses and any clinical outcomes.
Three studies (Tibballs and Russell 2009, 61; Tibballs and Weeranatna 2010, 671; Tsung and Blaivas 2007, 264) with 39 total patients and 376 pulse checks provided data on accuracy, with sensitivity ranging from 76 percent to 100 percent and specificity ranging from 64 percent to 79 percent. One study (Tibballs and Weeranatna 2010, 671) performed with children on left ventricular assist devices (LVADs) or extracorporeal membrane oxygenation (ECMO) reported that 60/153 (39 percent) of the participants decided on the presence of a pulse within 10 seconds, with a median duration until any decision of 18 seconds and accuracy of 85 percent. Although indirect, this evidence was concerning for prolonged chest compression pauses. No other studies were identified that assessed clinical outcomes in infants and children (Katzenschlager et al. 2024; Bray et al. 2025, S24).
A weak recommendation by ILCOR suggests that the palpation of a pulse (or its absence) is unreliable as the sole determinant of cardiac arrest and the need for chest compressions. In unresponsive children who are not breathing normally and who show no signs of life, lay rescuers and healthcare professionals should begin CPR (good practice statement). The following treatment recommendation has been withdrawn: In infants and children with no signs of life, healthcare providers should begin CPR unless they can definitely palpate a pulse within 10 seconds. In the justifications for the removal of this treatment recommendation, the authors again note that in one study (Tibballs and Weeranatna 2010, 671) only 39 percent (60/152) of participants decided on the presence of a pulse within 10 seconds (Katzenschlager et al. 2024; Scholefield et al. 2025, S116).
Insights and Implications
For lay responders, the Red Cross guidelines to begin CPR after confirming unresponsiveness and absent normal breathing remain unchanged. For healthcare providers, the withdrawal of the ILCOR recommendation for healthcare providers to check for a pulse is based largely on a single study to identify the presence or absence of a pulse in children with LVADs or on ECMO. The ILCOR recommendation that palpation of a pulse (or its absence) is unreliable as the sole determinant of cardiac arrest and the need for chest compressions suggests the need for additional studies comparing arterial blood pressure, alternative pulse check sites, ultrasound or ETCO2 changes combined with pulse checks versus pulse check alone in children with cardiac arrest. The Red Cross guidelines no longer recommend that healthcare professionals check a pulse in an unresponsive, apneic child, but allow consideration of a pulse check in select cases, such as a monitored inpatient who becomes unresponsive. If a healthcare professional does check a pulse in an unresponsive, apneic child, it should be limited to 10 seconds or less.
Duration of CPR Cycles
Last Full Review: ILCOR 2025
Last Update: 2014
Prolonged pauses during cardiopulmonary resuscitation (CPR) have been shown to be associated with lower odds for survival from ventricular fibrillation. This had led to studies evaluating survival and other patient outcomes when CPR is continued for longer periods before pausing for rhythm analysis. The International Liaison Committee on Resuscitation (ILCOR) systematic review on this topic was recently updated, leading to a fresh look at the Red Cross guidelines.
Red Cross Guidelines
- When feasible, chest compressions should be paused every 2 minutes for rhythm analysis and to allow for switching roles.
Evidence Summary
A 2025 ILCOR systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Smyth et al. 2024; Bray et al. 2025, S34) sought evidence to answer the following question: In adults and children in any setting with cardiac arrest, does pausing chest compressions at another interval compared with pausing chest compressions every 2 minutes to assess the cardiac rhythm change survival outcomes, return of spontaneous circulation (ROSC), coronary perfusion pressure or cardiac output?
This review was an update of a 2014 systematic review on the same topic. The search strategy led to the inclusion of two studies that were previously included in the 2014 ILCOR CoSTR (Nordseth et al. 2014, 75) or systematic review (Reynolds et al. 2015, 38). These studies were designed to address the provision of CPR first versus defibrillation first, and thus the evidence from this review was downgraded. The study by Wik et al. (Wik et al. 2003, 1389) assessed patients who received immediate defibrillation (up to 3 stacked shocks) followed by 3 minutes of CPR versus 1 minute of CPR for refractory ventricular fibrillation or ventricular tachycardia, and 3 minutes CPR for nonshockable rhythms. This study found no significant change in survival to hospital discharge with favorable neurological outcome, survival to hospital discharge or ROSC with 3 minutes of CPR versus 1 minute of CPR. The second included study (Baker et al. 2008, 424) evaluated patients enrolled in a separate randomized controlled trial (RCT) before implementation of new guidelines (i.e., with stacked shocks and 15:2 compression-to-ventilation ratio) who received 1 minute CPR cycles between shock sequences, compared with the control group enrolled in a separate RCT after implementation of new guidelines with single shocks, 30:2 CPR and 2 minute cycles between shocks. This study found no significant benefit for outcomes of survival to hospital discharge or ROSC with 1 minute of CPR versus 2 minutes of CPR.
The ILCOR treatment recommendation remains unchanged and suggests rescuers should assess the cardiac rhythm every 2 minutes (Smyth et al. 2024; Bray et al. 2025, S34).
Insights and Implications
Although the evidence for the current ILCOR treatment recommendation is quite limited and of low certainty, there was no evidence of potential benefit to be gained by changing the duration of CPR cycles, and there is value in being consistent with previous recommendations. The Red Cross guidelines have been updated to recommend that CPR should be paused after 2 minutes to allow for rhythm analysis and, when two or more responders are available, change of roles. This is consistent with recommendations related to provider fatigue and maintaining quality of CPR.
CPR Prior to Call for Help
Last Full Review: ILCOR 2020
Last Update: 2023
Mobile phones with audio command and speaker capability now make it possible to call 9-1-1 while simultaneously beginning cardiopulmonary resuscitation (CPR).
Red Cross Guidelines
- A mobile phone with a speaker, if available, should be used to call 9-1-1, allowing activation of emergency medical services to occur parallel to the beginning of cardiopulmonary resuscitation (CPR) and to facilitate dispatcher guidance and/or support of CPR.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council literature update did not identify any new relevant studies, and guidelines remain unchanged. This topic was last reviewed by the International Liaison Committee on Resuscitation in 2020 (Olasveengen et al. 2020, S41). The review included a single large cohort study of out-of-hospital cardiac arrest with CPR performed with dispatcher assistance identified from a national registry. Although a CPR-first strategy was not shown to improve survival to hospital discharge when compared with a call-first strategy, a subgroup analysis with adjusted data suggested a survival benefit with favorable neurological outcome using a CPR-first strategy, and a survival benefit with favorable neurological outcome was reported in patients under 20 years of age with use of a CPR-first strategy (aOR, 3.74; 95% CI, 1.46–9.61) (Olasveengen et al. 2020, S41).
Insights and Implications
This guideline reflects the technological changes in cell phone design, their widespread use and the ability to simultaneously call 9-1-1 using voice command while beginning CPR. This shifts the focus to initiating CPR as quickly as possible and helps avoid the need to leave a cardiac arrest victim to call 9-1-1.
Head-Up CPR
Last Full Review: ILCOR 2025
Last Update: 2023
Head-up cardiopulmonary resuscitation (CPR) is an emerging strategy that involves gradual elevation of the head after CPR has been initiated, and it has been shown in studies using cadaver and porcine models to improve cerebral blood flow and cerebral perfusion pressure when combined with active compression-decompression plus impedance threshold devices. A systematic review by the International Liaison Committee on Resuscitation (ILCOR) in 2021 included a single before-after observational study (Pepe et al. 2019, 449). This study suggested that augmented flow CPR through the addition of active compression-decompression with the use of an impedance threshold device, deferred positive pressure ventilations and gradual head and torso elevation may lead to improved short-term outcomes from cardiac arrest. However, there were limitations of the study that impacted the certainty of evidence. ILCOR made a weak recommendation suggesting against the routine use of head-up CPR and suggesting that the usefulness of this approach be assessed in clinical trials or research initiatives (Wyckoff et al. 2021, 229). Since 2021, some emergency medical services systems have developed protocols for the use of a head-up CPR bundle that includes an automated head/thorax-up positioning device, a mechanical CPR device and an impedance threshold device. In addition, new studies have been published, triggering an updated systematic review.
Red Cross Guidelines
- Head-up cardiopulmonary resuscitation should not be routinely used for cardiac arrest.
Evidence Summary
The 2025 ILCOR systematic review (Main et al. 2024, 100760) and Consensus on Science with Treatment Recommendations (CoSTR) (Norii et al. 2024; Bray et al. 2025, S24) evaluated evidence for the use of head-up CPR or a head-up CPR bundle (such as head-up position, active compression/decompression, use of impedance threshold devices) for adults and children in cardiac arrest in any setting compared with standard or compression-only CPR (CO-CPR) in a supine position. Critical outcomes of interest included survival at different stages and favorable neurological status. This was an update of the initial 2021 ILCOR systematic review (Wyckoff et al. 2021, 229). Three observational studies (Pepe et al. 2019, 449; Moore et al. 2022, 9; Bachista et al. 2024, 170) met inclusion criteria, all of which were included in the original 2021 systematic review. The study by Moore (Moore et al. 2022, 9) used data from the automated controller elevation-CPR (ACE-CPR) registry, while the Bachista study (Bachista et al. 2024, 170) used data from the automated head/thorax-up positioning-CPR (AHUP-CPR) registry. In the study by Pepe et al. (Pepe et al. 2019, 449), patients received either conventional (supine) CPR or head-up/torso-up CPR, both bundled with mechanical CPR and the use of an impedance threshold device. A “pit crew” approach was taken for rapid LUCAS® Chest Compression System placement, interrupting manual compressions for no more than 5 seconds. The head-up/torso-up CPR group underwent an initial priming period of supine CPR with oxygen administration but deferred positive pressure ventilations for several minutes. Patients were then gradually placed in a reverse Trendelenburg position at approximately 20 degrees after placement of the mechanical CPR device and with simultaneous placement of an advanced airway connected to an impedance threshold device. Data showed higher rate of return of spontaneous circulation (ROSC) to hospital arrival for out-of-hospital cardiac arrest (OHCA) treated with approximately 20 degree head-up CPR compared with the group treated with supine CPR (RR, 1.90; 95% CI, 1.61–2.26; P<0.001; aRR, 16.1%; 95% CI, 20.0%–12.2%) (Pepe et al. 2019, 449).
Moore et al. (Moore et al. 2022, 9) did not find a statistically significant difference for survival to hospital discharge following OHCA between the head-up CPR bundle of care group (227 adults) and the 5,196 adult patients who received conventional CPR in a supine position. Further analysis of odds ratio of cumulative survival to hospital discharge and hospital discharge with favorable neurological function was calculated based on the time between the 9-1-1 call to the start of head-up CPR for less than 20 minutes and from 20 to 38 minutes. There was no statistically significant difference between conventional CPR and head-up CPR groups (Moore et al. 2022, 9).
Bachista et al. (Bachista et al. 2024, 170) used data from 380 adult OHCAs who received the head-up bundle in the AHUP-CPR registry compared with 1,852 adult OHCAs with nonshockable rhythms who received conventional CPR in a supine position enrolled in two different randomized controlled trials (RCTs). Unadjusted data showed a greater likelihood of survival to hospital discharge in the head-up CPR group (7.4%, 28/380 versus 3.1%, 58/1,852). With propensity score matching, the likelihood of survival to hospital discharge increased further in the head-up CPR group (7.6%, 27/353 versus 2.8%, 10/353). For the outcome of survival with favorable neurological function, the head-up CPR bundle was associated with higher probabilities than with conventional CPR (4.2%, 15/353 versus 1.1%, 4/353; OR, 3.87; 95% CI, 1.27–11.78). However, in unadjusted analysis, rates of return of spontaneous circulation were not statistically different between the two groups (33% versus 29%) nor with adjusted analyses with propensity score matching (Bachista et al. 2024, 170).
The ILCOR treatment recommendation suggests against the use of head-up CPR or a head-up CPR bundle during CPR except in the setting of clinical trials of research initiative (Norii et al. 2024; Bray et al. 2025, S34). The review authors note the very low-certainty evidence that the head-up CPR bundle is associated with better survival and neurological outcomes. However, there are no RCTs evaluating the effect of head-up CPR or head-up CPR bundle. The studies to date have mainly evaluated a head-up CPR bundle with mechanical CPR with active compression-decompression and the use of an impedance threshold device. The optimal approach, including the angle and timing of head elevation, needs to be determined if head-up CPR proves to be beneficial.
Insights and Implications
One recent before-after observational study not included in the CoSTR evaluated end-tidal carbon dioxide (ETCO2) levels during head-up CPR or standard manual CPR on patients with OHCA, including all rhythms (Debaty et al. 2024, 110406). The study groups included 122 OHCA patients enrolled in a pre-intervention period where standard manual CPR was used and a 63-patient, post-intervention OHCA group where AHUP-CPR, active compression-decompression CPR and an impedance threshold device (ITD-16) was used. Baseline ETCO2 values were comparable between the two groups, but during CPR, the head-up CPR group’s ETCO2 values were significantly higher than the conventional CPR group (40.7 millimeters of mercury (mmHg) versus 30.3 mmHg) and approached physiologic levels, regardless of the presenting rhythm. However, all clinical survival outcomes did not differ between the two groups (Debaty et al. 2024, 110406).
The ILCOR review makes important points about the lack of any RCTs and the lack of studies to determine an optimal angle and timing of head elevation. In addition, the equipment to provide a head-up CPR bundle and the necessary training is expensive and requires additional resources. Transitioning a person in cardiac arrest from supine to a head-up position is logistically challenging and may create interruptions in delivery of compressions. If manual compressions are used in a head-up position, they may be less effective than mechanical CPR devices or compressions delivered to a person in the supine position. Head-up CPR is promising but requires further research.
CPR Prior to Defibrillation
Last Full Review: ILCOR 2020
Last Update: 2024
The optimal time to perform cardiopulmonary resuscitation (CPR) prior to defibrillation is unclear.
Red Cross Guidelines
- Cardiopulmonary resuscitation should be performed prior to the availability of an automated external defibrillator and analysis of rhythm.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council literature update did not identify any new human studies evaluating CPR intervals prior to defibrillation, and the guidelines remain unchanged. This topic was last reviewed systematically by the International Liaison Committee on Resuscitation in 2020 (Olasveengen et al. 2020, S41) without evidence of a clear survival benefit for out-of-hospital cardiac arrest following a prolonged period of CPR compared with a shorter period of CPR prior to defibrillation.
Insights and Implications
The ideal time to perform CPR on adults and children with a shockable rhythm following out-of-hospital cardiac arrest remains a knowledge gap, but this time should not be extended beyond the arrival of an automated external defibrillator, turning the power on and applying the defibrillator pads.
Optimal Surface for Performing CPR
Last Full Review: American Red Cross Scientific Advisory Council 2021 (Layperson); ILCOR 2020 (Inpatient)
Last Update: 2024
Recommendations from a 2019 International Liaison Committee on Resuscitation (ILCOR) systematic review (Olasveengen et al. 2020, S41) and an American Red Cross Scientific Advisory Council Answer in 2021 suggest performing chest compressions on a firm surface when possible. For in-hospital cardiac arrest, the use of the cardiopulmonary resuscitation (CPR) mode is suggested, when available, to increase hospital bed mattress stiffness, and it is suggested against moving a patient from a bed to the floor to improve chest compression depth. The American Red Cross Scientific Advisory Council review addressed concerns raised about a layperson moving a person in out-of-hospital cardiac arrest from the bed to the floor due to the potential for injury to both the lay responder and the person in cardiac arrest, and a concern for the inherent delay in initiating chest compressions.
Red Cross Guidelines
- It is reasonable to perform manual chest compressions on a firm surface when this is practical and does not significantly delay the commencement of chest compressions in adults, children and infants.
- It is suggested that a person in cardiac arrest in the hospital setting not be moved from their bed to the floor to improve chest compression depth.
- If a person in cardiac arrest is in a bed with cardiopulmonary resuscitation mode to increase mattress stiffness, it is reasonable to activate this mode.
Evidence Summary
An ILCOR systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Dewan et al. 2024, 100718; Dewan et al. 2024; Greif et al. 2024), updated in 2023, evaluated new evidence for adults and children in cardiac arrest comparing the performance of CPR on a hard surface with CPR on a regular mattress or other soft surface. Both clinical and CPR quality outcomes were sought. Six additional manikin randomized controlled trials (RCTs) and one observational study were included in the updated review. The updated meta-analysis for CPR on a backboard compared with a hospital mattress included seven adult manikin RCTs, showing a mean difference in compression depth of 2.16 millimeters (mm) (95% CI, 0.52–3.81), while data from five adult manikin RCTs showed a mean difference in compression rate of -0.11 (95% CI, -3.8–3.59) (Dewan et al. 2024; Greif et al. 2024).
For the updated meta-analysis of data for CPR performed on the floor compared with a hospital mattress, data from two adult manikin RCTs showed a compression depth mean difference of -5.36 mm (95% CI, -1.59–12.32). The updated meta-analysis of data for CPR performed on the floor compared with a firm (home) mattress included two adult manikin RCTs and showed a compression depth mean difference of 2.11 mm (95% CI, -3.23–7.45) (Dewan et al. 2024; Greif et al. 2024).
Although the mean difference in compression depth achieved by moving to a firm surface was very small in this systematic review, overall, compression depth was inadequate, with most studies failing to reach the recommended depth of greater than 50 millimeters.
The updated ILCOR treatment recommendations include:
- A weak recommendation for performing chest compressions on a firm surface when this is practical and does not significantly delay the commencement of chest compressions.
- A good practice statement suggesting activation of the CPR mode to increase mattress stiffness, if available, for in-hospital cardiac arrest.
- For healthcare systems that have already incorporated backboards into routine use during resuscitations, the evidence was considered insufficient to suggest against their continued use.
- A weak recommendation for healthcare systems that have not introduced backboards: The limited improvement in compression depth and uncertainty about harm seemed insufficient to justify the costs of purchasing backboards and training staff in their use.
The most recent American Red Cross Scientific Advisory Council Answer (American Red Cross Scientific Advisory Council 2023b) for this topic considered delay in starting CPR, as well as the potential for injury to both the lay responder and the patient in cardiac arrest should the patient need to be moved from a mattress to the floor. The lay responder in this setting is typically a sole family member who may need to lift or drag a much heavier family member off a home mattress to the floor, risking injury to the patient as well as themselves. This process also takes time, causing a delay in starting CPR. Two identified manikin studies (Ahn et al., 2021, 37; Missel et al. 2023, 691) simulated CPR in the out-of-hospital setting, where beds may be softer than hospital beds, and one study simulated a single, untrained rescuer (Missel et al. 2023, 691). One study (Ahn et al., 2021, 37) reported lower median CPR rates when CPR was performed on a soft home mattress, and less self-reported fatigue when CPR was performed on the floor compared to a mattress. The RCT by Missel (Missel et al. 2023, 691) evaluated CPR performance on manikins by participants without professional healthcare training, reporting that compression depth was less than the 5-to-6 centimeter depth recommended for adults when performed on both a mattress and the floor. In addition, mean compression depth was greater with the manikin on the floor than on the mattress, and less for female participants. No studies have directly assessed the logistics and impact of moving a person to the floor in an out-of-hospital setting.
Insights and Implications
There continues to be a lack of human studies that evaluate outcomes related to CPR performed on different surfaces, and there are few studies that include pediatric patients or manikins. The ILCOR update now considers the potential risks of harm, including interruption in CPR, and harm to the patient and lay provider or resuscitation team member when moving a patient to the floor, which outweigh any minimal improvement in chest compression depth.
While this evidence is very limited, it continues to support current Red Cross guidelines. It may be more difficult to meet the recommended compression depth and rate when performing CPR on a soft home mattress, but the risk of injury to the patient in cardiac arrest, the risk of injury to the lay provider attempting the move, and the delay or interruption in CPR must be weighed in each situation. The revision to the Red Cross guidelines to perform manual chest compressions on a firm surface when this is practical and does not significantly delay the commencement of chest compressions, reflects the need to balance the advantages of moving a person in cardiac arrest from a mattress or recliner against the delay in starting CPR and risk of injury to the lay rescuer and the patient. Although there is little to no research focused on pediatric patients, it should be logistically easier to move a child or infant to a firm surface, when needed. Additional research is needed particularly for layperson CPR and with consideration of single versus two or more available bystanders to assist with a movement to a firm surface.
Barrier Devices During CPR
Last Full Review: American Red Cross Scientific Advisory Council 2021; ILCOR 2020
Last Update: 2022
Barrier devices used during cardiopulmonary resuscitation (CPR) include face masks, face shields and surgical masks. The coronavirus disease 2019 (COVID-19) pandemic led to a greater use of these devices to protect rescuers from infectious disease transmission. Is there additional evidence to show the efficacy of various barrier devices from transmitting infectious disease?
Red Cross Guidelines
Although the risk of harm while performing cardiopulmonary resuscitation is considered low, precautions should be taken to minimize the risk of transmission of infectious disease. This may include, but is not limited to:
- Using standard precautions to provide patient care in all settings including performance of hand hygiene and use of personal protective equipment (PPE), that is, gloves, gown and a face mask, based on activities being performed and the risk assessment.
- Using additional PPE, including an N95 or higher-level respirator and eye protection (goggles or face shield) for aerosol-generating procedures or resuscitation of patients. Disposable N95 respirators should be discarded after leaving the patient’s room or care area.
- Using an inline filter for mouth-to-mask or bag-mask ventilation.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council scientific review (American Red Cross Scientific Advisory Council: First Aid 2021a) evaluated the risk of infection during CPR and first aid. Case reports identified in this review document the transmission of a variety of infectious diseases during resuscitation. In most cases, personal protective equipment (PPE) in the form of gloves or a barrier device for rescue breathing were not used. A 2022 evidence update (Wyckoff et al. 2022, e483) of a 2005 Consensus on Science with Treatment Recommendations (International Liaison Committee on Resuscitation 2005, 187) by the International Liaison Committee on Resuscitation (ILCOR) searched for evidence related to the use of barrier devices, compared with no use of barrier devices by rescuers performing CPR on adult or pediatric patients for out-of-hospital cardiac arrest and in-hospital cardiac arrest. Outcomes of interest included lower infection rates and quality of ventilation. No new studies were identified that were specifically related to barrier devices during CPR since a previous 2020 ILCOR evidence update and a systematic review (Couper et al. 2020, 59) of COVID-19 in cardiac arrest and infection risk to rescuers. The previous ILCOR treatment recommendation remains unchanged and recommends that providers should take appropriate safety precautions when feasible and when resources are available to do so, especially if a victim is known to have a serious infection (e.g., human immunodeficiency virus, tuberculosis, hepatitis B virus or severe acute respiratory syndrome) (Wyckoff et al. 2022, e483).
Insights and Implications
There are relatively few reports of infectious disease transmission following the provision of CPR. Despite the lack of evidence beyond case series showing an association between chest compressions or defibrillation and transmission of COVID-19 to rescuers, lay responders and healthcare professionals can proactively reduce any risk through the use of PPE, when available, including the use of barrier devices.
CPR Start Sequence (A-B-C versus C-A-B) for Adults and Pediatric Patients
Last Full Review: ILCOR 2025
Last Update: 2023
Current guidelines for adults recommend beginning cardiopulmonary resuscitation (CPR) with chest compressions before ventilations. Starting CPR with chest compressions has been shown to lead to faster times to delivery of compressions, rescue breaths and other elements of resuscitation. For children and infants, because cardiac arrest is usually preceded by a respiratory event, the Red Cross recommends starting CPR with rescue breaths or ventilations before compressions. A 2025 updated review by the International Liaison Committee on Resuscitation (ILCOR) evaluates strategies for starting CPR.
Red Cross Guidelines
- Once cardiac arrest is recognized, resuscitation should begin with compressions.
- For infants and children with cardiac arrest due to a suspected respiratory etiology, healthcare professionals and those with a duty to respond may consider beginning CPR with rescue breaths or manual ventilations.
- Healthcare professionals and laypersons should provide rescue breaths or manual ventilations with compressions in pediatric patients with out-of-hospital cardiac arrest.
- For the drowning process resuscitation, once cardiac arrest is recognized, resuscitation should begin with rescue breaths or manual ventilations.
Evidence Summary
An ILCOR systematic review updated in 2025 (Bray et al. 2025 ILCOR; Bray et al. 2025, S34) sought clinical outcomes and CPR metrics in adults and children with in-hospital cardiac arrest or out-of-hospital cardiac arrest who receive CPR beginning with compressions (30 compressions to 2 ventilations) compared with beginning with ventilations (2 ventilations to 30 compressions). Studies of dispatcher- or telecommunicator-assisted CPR were excluded. No studies with human subjects were identified, and data from a single pediatric manikin study was added to evidence from four manikin simulation studies found in the previous ILCOR systematic review.
In summary, a compression-first approach was shown to decrease the time to starting chest compressions in a cardiac arrest scenario, while the mean time to providing ventilations was longer. One randomized study (Lubrano et al. 2012, 1473) from the previous systematic review used a simulated pediatric respiratory arrest scenario. The study reported that ventilation was started earlier with a compression-first approach versus a ventilation-first approach (mean 19.1 plus or minus 1.5 seconds versus 22.7 plus or minus 0.1 seconds, P<0.05). Other important outcomes from the ILCOR review included:
- A shorter mean time to completion of the first resuscitation cycle (30 compressions to 2 ventilations) with a compression-first approach (Marsch et al. 2013, w13856).
- A higher median number of ventilations given in the first minute with an A-B-C approach that included 5 initial rescue breaths (one study, simulated pediatric resuscitation) (Suppan et al. 2022, 1799).
- A lower chest compression fraction with a 5-rescue-breaths or ventilations-first approach in one simulated pediatric resuscitation study (Suppan et al. 2022, 1799; Suppan et al. 2023, 1799 published with corrections) compared to no difference in a second simulated adult resuscitation study (Kobayashi et al. 2008, 333).
- A higher alveolar ventilation in the first minute of resuscitation with a 5-rescue-breaths A-B-C approach in a simulated pediatric resuscitation study (Suppan et al. 2022, 1799).
The ILCOR treatment recommendation for adults suggests commencing CPR in cardiac arrest with compressions rather than ventilations (Bray et al. 2025 ILCOR; Bray et al. 2025, S34).
In consideration of the evidence evaluation for children and infants, most studies used manikins and findings suggested that starting CPR with compressions results in beneficial elements of resuscitation, such as higher alveolar ventilation volumes, during the first minute of resuscitation (Suppan et al. 2022, 1799; Kobayashi et al. 2008, 333; Marsch et al. 2013, w13856; Sekiguchi et al. 2013, 1248; Lubrano et al. 2012, 1473). One simulated pediatric resuscitation study (Lubrano et al. 2012, 1473) found that starting CPR with compressions delayed commencement of rescue breaths in cardiac arrest by 6 seconds. Although this delay may be clinically acceptable, it was also noted that alveolar minute ventilation and the number of ventilations delivered in the first minute of resuscitation were higher with the A-B-C approach that included delivering 5 rescue breaths before starting compressions. The ILCOR Pediatric Life Support Task Force concluded that there is insufficient evidence to support a treatment recommendation regarding the optimal order of commencing CPR in children (ventilations or compressions first) (Bray et al. 2025 ILCOR; Bray et al. 2025, S34).
The International Liaison Committee on Resuscitation provided a good practice statement that both an A-B-C approach (ventilation followed by compression) and a C-A-B approach (compressions followed by ventilation) are acceptable, and both ventilation and chest compressions are important components of CPR in children (Bray et al. 2025 ILCOR; Bray et al. 2025, S34).
Insights and Implications
The Red Cross guidelines continue to recommend starting CPR in adults, children and infants with compressions rather than ventilations. Advantages to starting CPR with compressions extend beyond faster times to starting chest compressions, starting and completing the first cycles of chest compressions, and a higher compression fraction. Coronary perfusion pressure is dependent on effective chest compressions during cardiac arrest, and time to the first compression is associated with better clinical outcomes in adults. Recommending an A-B-C approach for bystanders could potentially lead to no provision of CPR when there are concerns over providing mouth-to-mouth ventilations, or it could lead to delays in starting CPR when searching for a pocket mask or a bag-valve-mask device.
For infants and children, however, there are no clinical studies and only a few simulation studies using manikins. One can argue for or against starting CPR with ventilations. Based on this updated ILCOR systematic review, the Red Cross guidelines continue to suggest that healthcare professionals as well as those with a duty to respond (lifeguards, police and firefighters) may consider providing rescue breaths or manual ventilations first in pediatric patients with suspected primary respiratory etiologies of cardiac arrest. In addition, it should be noted that the guidelines for starting CPR do not alter the existing guidelines specifically for drowning beginning resuscitation with rescue breaths or ventilations. (See Drowning Process Resuscitation.)
Chest Compression Rate
Last Full Review: ILCOR 2020
Last Update: 2023
Is there a chest compression rate during cardiopulmonary resuscitation (CPR) that is associated with higher rates of survival to hospital discharge with or without good neurological outcome?
Red Cross Guidelines
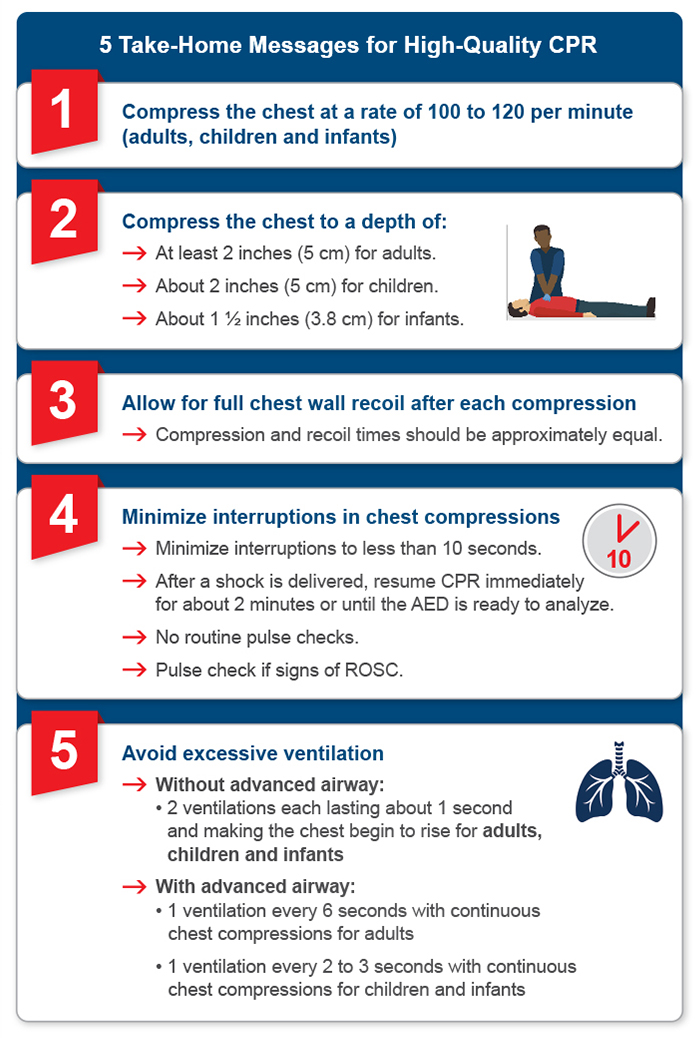
- Chest compressions should be performed at a rate of 100 to 120 per minute for adults, children and infants.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council literature update on chest compression rate during CPR did not identify new relevant studies since January 2020 and guidelines remain unchanged. Evidence for chest compression rates used in CPR was last reviewed systematically in 2015 by the International Liaison Committee on Resuscitation, (Travers et al. 2015, S51) followed by a scoping review in 2020 (Olasveengen et al. 2020, S41; Considine et al. 2020, 188).
The 2015 systematic review included large observational studies showing an association between increasing chest compression rates and declining chest compression depth, and a decrease in survival to hospital discharge with compression rates above 140 per minute (International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Part 2 2005, 187). A strong treatment recommendation was made for a manual chest compression rate of 100 to 120 per minute. The more recent scoping review (Olasveengen et al. 2020, S41; Considine et al. 2020, 188) of chest compression rate, depth and chest wall recoil identified additional observational studies and one randomized controlled trial evaluating chest compression rate; some studies evaluated compression rate in isolation, and others in conjunction with compression depth. Several studies suggested confounding interactions and advised caution when evaluating any chest compression component in isolation. The review concluded that there was insufficient evidence to support a new systematic review or change to treatment recommendations (Olasveengen et al. 2020, S41).
Insights and Implications
The chest compression rate is defined as the rate used for each continuous period of chest compressions over 1 minute, excluding pauses (Travers et al. 2015, S51). Studies evaluating chest compression rate are primarily observational, from the out-of-hospital cardiac arrest setting, and do not account for potential interactions from compression depth, hand position and other components of chest compression. More recent studies of compression rate have focused on rescuer fatigue with compressions, use of automatic compression devices compared with manual compression, and real-time CPR feedback devices to help maintain correct compression rates and quality of chest compression.
Chest Compression Depth
Last Full Review: ILCOR 2020
Last Update: 2023
Is there a compression depth during cardiopulmonary resuscitation (CPR) that is associated with higher rates of survival to discharge with or without good neurological outcome?
Red Cross Guidelines
-
During cardiopulmonary resuscitation (CPR), an adult chest should be compressed to a depth of at least 2 inches.
- During CPR, a child’s and infant’s chest should be compressed to a depth of at least one-third the anteroposterior diameter of the chest (about 2 inches for a child and about 1 1/2 inches for an infant).
Evidence Summary
No new relevant studies of chest compression depth during CPR were identified by American Red Cross Scientific Advisory Council in a 2021 literature update, and the guidelines remain unchanged. Evidence for chest compression depth during CPR was last reviewed systematically in 2015 by International Liaison Committee on Resuscitation (ILCOR), (Travers et al. 2015, S51) followed by a scoping review in 2020 (Olasveengen et al. 2020, S41; Considine et al. 2020, 188).
The 2015 ILCOR systematic review (Travers et al. 2015, S51) led to a strong treatment recommendation for a manual chest compression depth of approximately 2 inches (5 centimeters) in adults, and a weak recommendation was made for avoiding excessive chest compression depths (greater than 2.4 inches [6 centimeters] in an average adult). The upper limit for chest compression depth reflected evidence suggesting that a depth of more than 2.4 inches is associated with a higher rate of injuries in adults compared with a depth of 2 inches to 2.4 inches (5 centimeters to 6 centimeters). The more recent scoping review (Olasveengen et al. 2020, S41; Considine et al. 2020, 188) identified observational studies evaluating both chest compression rate and depth as well as one randomized controlled trial and several observational studies evaluating depth alone. There was insufficient new evidence to support a systematic review or reconsideration of ILCOR treatment recommendations (Olasveengen et al. 2020, S41).
Insights and Implications
Studies evaluating compression depth in isolation are commonly confounded by many factors, including body and chest size, as well as chest wall compliance. Studies identified but excluded in the American Red Cross Scientific Advisory Council literature update focus on other factors that may impact compression depth including:
-
Leaning on the chest.
-
Kneeling on a bed to deliver compressions.
-
Rescuer height and weight.
-
Firmness of surfaces under a body.
-
Use of mechanical compression devices versus manual compression.
-
Compression cycle length.
- Use of real-time feedback devices.
Future guidance will likely reflect some of these factors as new studies emerge.
Chest Wall Recoil
Last Full Review: ILCOR 2020
Last Update: 2023
Chest wall recoil allows the chest to return to its normal position following a chest compression, allowing for venous return to the heart. Leaning on the chest wall between compressions restricts recoil and can increase intrathoracic pressure and reduce right heart filling and coronary perfusion pressure. Does maximizing chest wall recoil improve return of spontaneous circulation and clinical outcomes?
Red Cross Guidelines
- During compressions for adults, children and infants, the chest wall should be allowed to fully recoil, and compression and recoil times should be approximately equal.
Evidence Summary
Evidence for chest wall recoil during cardiopulmonary resuscitation (CPR) was the subject of a 2021 American Red Cross Scientific Advisory Council literature update and was last reviewed systematically in 2015 by International Liaison Committee on Resuscitation (ILCOR), (Travers et al. 2015, S51) followed by a scoping review in 2020 (Olasveengen et al. 2020, S41; Considine et al. 2020, 188).
The 2021 American Red Cross Scientific Advisory Council literature update identified one recent randomized simulation trial that reported an association between rescuers’ height and weight and the chest compression depth and recoil (Bibl et al. 2020, 1831). An older simulation study also reported an association between higher weight and body mass index, male sex and height, and a lower likelihood to achieve a complete chest wall recoil (Contri et al. 2017, 1266). Other studies focus on the impact of real-time CPR feedback devices and rescuer physical fitness when providing CPR. These studies do not support a change in guidelines.
The 2015 systematic review (Travers et al. 2015, S51) by ILCOR included evidence from two animal studies and one observational study in anesthetized children not in cardiac arrest, all reporting reduced coronary perfusion pressure with incomplete chest wall recoil. The pediatric study applied a force on the chest corresponding to 10 percent to 20 percent of body weight, with the finding of a proportional reduction in coronary perfusion pressure, but without effect on cardiac output (Travers et al. 2015, S51).
The 2020 ILCOR scoping review (Considine et al. 2020, 188; Olasveengen et al. 2020, S41) did not identify new studies of chest wall recoil, while a 2022 evidence update (Berg et al., 2023) noted four new observational studies with findings reported as consistent with current guidelines
Insights and Implications
Chest wall recoil allows the chest to return to its normal position following a chest compression, allowing for venous return to the heart. Leaning on the chest wall between compressions is common and restricts recoil, increasing intrathoracic pressure and reducing right heart filling and coronary perfusion pressure. The limitedevidence supports full chest wall recoil between chest compressions to improve CPR quality. Factors impacting chest wall recoil include the release or recoil velocity, release time and release height. Release or recoil velocity is the maximum velocity during the recoil phase, has been reported to be independently associated with improved survival and favorable neurologic outcomes at discharge following out-of-hospital cardiac arrest (Kovacs et al. 2015, 107), while a benefit was not shown in another study using adjusted data (Cheskes et al., 2016, 253). Although recoil velocity has been proposed as a future quality metric for CPR, further research is needed to define its impact on survival from cardiac arrest.
Hand Positioning During Chest Compressions
Last Full Review: ILCOR 2025
Last Update: 2020
Effective chest compressions during cardiopulmonary resuscitation (CPR) require proper hand placement on the chest, an adequate compression depth, a correct compression rate and other components such as full chest recoil. Historically, the recommended location for placing hands on a person’s chest was “over the lower half of the victim’s sternum” which was accomplished by instructing the student to place the heel of their hand in the center of the chest with the other hand on top. The International Liaison Committee on Resuscitation (ILCOR) first reviewed this topic in 2010 (Sayre et al. 2010, S298). Determining the ideal position for producing effective compressions and teaching how to identify a proper location is challenging and has been studied with use of computed tomography, echocardiography and manikin studies.
An updated ILCOR review in 2020 (Olasveengen et al. 2020, S41) included studies evaluating physiological endpoints with compressions over the lower third of the sternum compared with the center of the chest or middle of the sternum. Recommendations for performing chest compressions on the lower half of the sternum in adults in cardiac arrest were unchanged from the 2015 review. This topic was reviewed again for 2025.
Red Cross Guidelines
- For adults and children, chest compressions should be performed on the lower half of the sternum.
- In children 1 to 8 years of age, it is reasonable to compress with one hand (heel of palm on child’s sternum), or to use two hands to perform compressions (heel of one palm on child’s sternum with other hand on top). Careful attention should be paid to adequate depth of at least one-third the anteroposterior depth of the chest (approximately 2 inches or 5 centimeters).
- In infants up to 1 year of age, it is reasonable to perform compressions with two thumbs/encircling hands or with the heel of one palm on the infant’s sternum. Careful attention should be paid to adequate depth of at least one-third the anteroposterior depth of the chest (approximately 1.5 inches or 4 centimeters).
Evidence Summary
A 2025 updated ILCOR systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Raffay et al. 2024; Bray et al. 2025, S34) evaluated evidence for the delivery of chest compressions to adults and children in cardiac arrest in any other location compared with delivery of compressions on the lower half of the sternum. Imaging studies were excluded from the current review. No studies were identified that reported clinical outcomes such as return of spontaneous circulation or survival. Two crossover studies in adults with cardiac arrest provided physiologic data (Cha et al. 2013, 691; Qvigstad et al. 2013, 1203). Cha et al. (Cha et al. 2013, 691) reported higher peak arterial pressure during compressions systole and higher end-tidal carbon dioxide levels (ETCO2) when compressions were performed over the lower third of the sternum versus the center of the chest. However, coronary perfusion pressure and other indices did not differ. Qvigstad et al. (Qvigstad et al. 2013, 1203) did not find a difference between ETCO2 values and hand placement. One small crossover study in children (Orlowski et al. 1986, 667) reported higher peak systolic blood pressure and mean arterial blood pressure with compressions over the lower third of the sternum versus the middle of the sternum. The ILCOR CoSTR continues to suggest performing chest compressions over the lower half of the sternum for adults in cardiac arrest (Raffay et al. 2024; Bray et al. 2025, S24).
Insights and Implications
Although the recommended location for hand placement to deliver chest compressions remains the lower half of the sternum, the ILCOR systematic review authors noted that imaging studies excluded from the review examined hand position for chest compressions and indicated that for most adults and pediatric patients, the maximal ventricular cross-sectional area underlies the lower third of the sternum/xiphisternal junction (Raffay et al. 2024; Bray et al. 2025, S34). However, some studies suggest that there may be important anatomic variations in the population based on age, body mass index, pregnancy, preexisting congenital cardiac disease, and so on. A single specific location for hand placement to deliver chest compressions may not be optimal for every person. Thus, in the absence of clinical data, the ILCOR treatment recommendation and Red Cross guidelines remain unchanged. Hand positioning and technique for CPR in infants and neonates are addressed separately in the healthcare guidelines database. (See Neonatal Advanced Life Support: CPR Techniques and Process.)
Minimizing Pauses in Chest Compressions
Last Full Review: ILCOR 2022
Chest compression fraction (CCF) is the proportion of time spent providing chest compressions during cardiopulmonary resuscitation (CPR) and is measured by dividing the cumulative time spent providing chest compressions by the total time taken for the entire resuscitation. The interruption of chest compressions during CPR to perform rescue breaths, rhythm analysis, pulse checks and defibrillation all reduce chest compression fraction, leading to decreased coronary and cerebral blood flow and the potential for decreased survival (Aramendi and Irusta 2016, E121). A CCF of greater than 80 percent is considered a high-quality CPR metric. This has led to efforts to minimize the frequency and duration of peri-shock pauses, to provide continuous chest compressions without pauses for ventilations and the development of artifact-filtering algorithms in automated external defibrillators (AEDs). Is there new evidence to support efforts to minimize pauses in chest compressions?
Red Cross Guidelines
- Pauses during cardiopulmonary resuscitation, including peri-shock pauses, changing roles, and moving between ventilations and compressions for a single rescuer, should be as short as possible.
- Chest compression fraction (CCF) should be as high as possible and at least 60 percent.
- Where system resources permit, monitoring of peri-shock pauses and CCF may be considered as part of a comprehensive quality improvement program.
Evidence Summary
A systematic review and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2022, e483; Olasveengen et al. 2022) by International Liaison Committee on Resuscitation updated in 2022 evaluated the evidence for minimizing pauses in chest compressions in adults in cardiac arrest in any setting (i.e., a higher CPR fraction or chest compression fraction, or shorter peri-shock pauses), compared with conventional CPR (with a lower CPR or chest compression fraction, or longer peri-shock pauses). The review included several observational studies and three randomized controlled trials (RCTs) (Jost et al. 2010, 1614; Beesems et al. 2016, 1; Rea et al. 2014, 879). The overall certainty of evidence across outcomes was rated as very low. Meta-analyses were not possible due to confounding and a high degree of heterogeneity. Of the included RCTs, one trial (Jost et al. 2010, 1614) using an experimental AED algorithm observed higher CCFs and shorter pre-shock and post-shock pauses, with no significant difference in survival to hospital admission or hospital discharge when compared to the control group. A second trial (Nichol et al. 2015, 2203) observed a higher CCF in a continuous chest compression group compared with 30:2 compression-ventilation CPR, with lower survival to hospital admission but no difference in survival to hospital discharge. A third trial (Beesems et al. 2016, 1) using an experimental AED algorithm observed a higher CCF and shorter pre-shock and post-shock pauses compared with the control group, but no significant differences in survival to hospital admission or hospital discharge (Wyckoff et al. 2022, e483; Olasveengen et al. 2022). 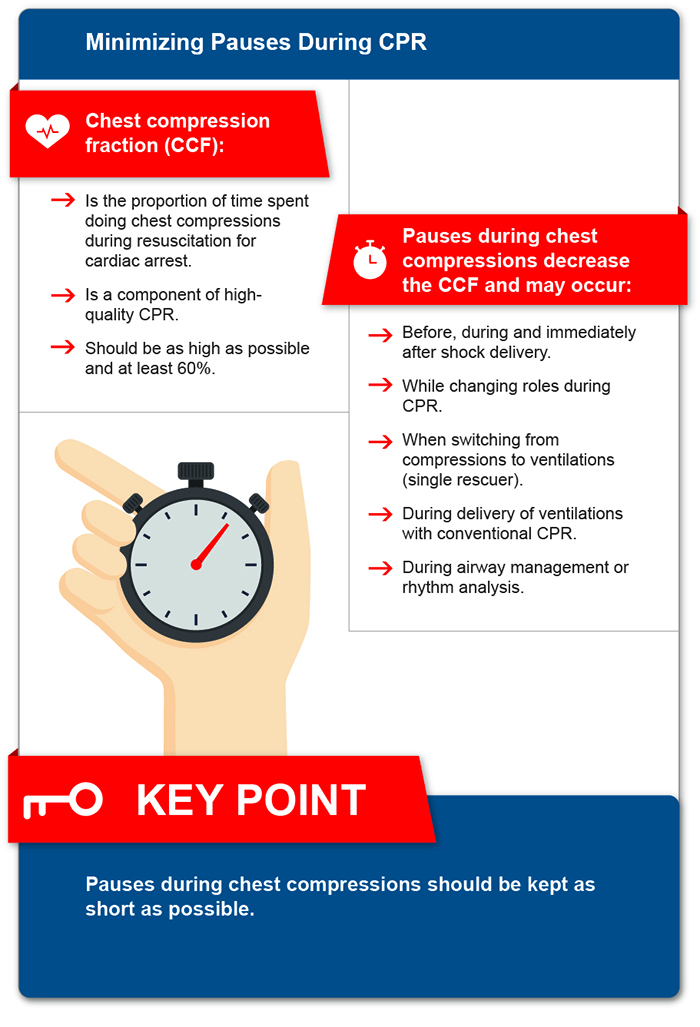 The included observational studies evaluated outcomes following incremental changes in CPR quality metrics and outcomes over time, outcomes for patients treated in physician-staffed versus paramedic-staffed ambulances, and outcomes following training and feedback interventions. While increases in CCF and/or shorter peri-shock pauses were documented with these interventions, most studies reported no significant differences for survival to hospital discharge. One observational study (Rea et al. 2014, 879) reported higher survival for cardiac arrest with a CCF greater than 80.4 percent compared with less than 80.4 percent in a subgroup with a 20-minute CPR duration. Two other studies reported higher adjusted odds ratio for survival with a lower CCF compared with higher CCFs while other studies reported no significant difference in outcomes (Wyckoff et al. 2022, e483; Olasveengen et al. 2022). For peri-shock pauses, most observational studies reported higher survival in patients with shorter pre-shock pauses (less than 10 seconds) compared with longer pauses (greater than 10 to 20 seconds), and a few reported higher survival in patients with shorter peri-shock pauses (less than 20 seconds) compared with longer pauses (greater than 20 to 40 seconds). In adjusted analysis, the most recent study enrolling 15,568 patients did not report higher odds of survival with shorter pre-shock pauses (less than 10 seconds) compared with longer pauses (greater than 10 seconds) (Cheskes et al. 2017, 39). Divergent results were reported in observational studies in which pauses in compressions were compared between survivors and nonsurvivors of out-of-hospital cardiac arrest (Wyckoff et al. 2022, e483; Olasveengen et al. 2022).
The included observational studies evaluated outcomes following incremental changes in CPR quality metrics and outcomes over time, outcomes for patients treated in physician-staffed versus paramedic-staffed ambulances, and outcomes following training and feedback interventions. While increases in CCF and/or shorter peri-shock pauses were documented with these interventions, most studies reported no significant differences for survival to hospital discharge. One observational study (Rea et al. 2014, 879) reported higher survival for cardiac arrest with a CCF greater than 80.4 percent compared with less than 80.4 percent in a subgroup with a 20-minute CPR duration. Two other studies reported higher adjusted odds ratio for survival with a lower CCF compared with higher CCFs while other studies reported no significant difference in outcomes (Wyckoff et al. 2022, e483; Olasveengen et al. 2022). For peri-shock pauses, most observational studies reported higher survival in patients with shorter pre-shock pauses (less than 10 seconds) compared with longer pauses (greater than 10 to 20 seconds), and a few reported higher survival in patients with shorter peri-shock pauses (less than 20 seconds) compared with longer pauses (greater than 20 to 40 seconds). In adjusted analysis, the most recent study enrolling 15,568 patients did not report higher odds of survival with shorter pre-shock pauses (less than 10 seconds) compared with longer pauses (greater than 10 seconds) (Cheskes et al. 2017, 39). Divergent results were reported in observational studies in which pauses in compressions were compared between survivors and nonsurvivors of out-of-hospital cardiac arrest (Wyckoff et al. 2022, e483; Olasveengen et al. 2022).
Insights and Implications
High-quality CPR is important for patient outcomes and includes the provision of chest compressions for at least 60 percent and up to or more than 80 percent of the entire resuscitation. To achieve this CCF, it is necessary to minimize pauses that can occur with interventions, such as intubation and peri-shock pauses. While this systematic review did not find strong evidence of a survival benefit with higher CCFs and decreased peri-shock pauses, the review authors noted that observational studies of pauses in compressions are challenging to interpret because short duration resuscitation efforts in patients with shockable rhythms tend to have better outcomes than long duration resuscitation efforts in patients with non-shockable rhythms. The cardiac rhythm and the duration of resuscitation will impact the number and duration of pauses. This makes it difficult to determine optimal pause duration or frequency for guidance, although it is unlikely that a reduction in the frequency and duration of pauses will produce harmful effects. Technological advances with the development of algorithms to automatically detect chest compression periods using an accelerometer may allow for future automated CCF calculations, monitoring and research.
Pulse Check During CPR
Last Full Review: American Red Cross Scientific Advisory Council 2015; ILCOR 2015
Last Update: 2023
Chest compression fraction (CCF) is the amount of time during cardiac arrest in which chest compressions are administered and may be calculated manually or by automated external defibrillator analytic software that permits identification of all interruptions greater than 2 seconds. Any interruption in chest compressions during cardiopulmonary resuscitation (CPR), such as for a pulse check, can contribute to a reduced CCF. Does interruption of CPR to perform a pulse (circulation) check, compared with no interruption of CPR, change outcomes, including return of spontaneous circulation (ROSC), survival or CCF?
Red Cross Guidelines
- When performing cardiopulmonary resuscitation (CPR), if signs of return of spontaneous circulation (ROSC) are observed:
- Stop CPR and automated external defibrillator use.
- Check for breathing and a carotid or femoral pulse.
- Pauses should be minimized to less than 10 seconds.
- Routine pulse checks without signs of ROSC return of spontaneous circulation are not recommended.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council literature update did not identify studies to support routine pulse checks during CPR for basic life support. A 2015 American Red Cross Scientific Advisory Council scientific review and a 2015 International Liaison Committee on Resuscitation systematic review (Travers et al. 2015, S51) did not identify human studies specific to this question. The 2021 American Red Cross Scientific Advisory Council literature update identified studies in monitored situations related to the use of a doppler and end-tidal capnography and electrocardiogram morphology as a means of confirming pulse or ROSC. While these technologies may be useful in identifying ROSC in a monitored, advanced life support setting, there continues to be no evidence to support routine pulse checks during CPR for basic life support.
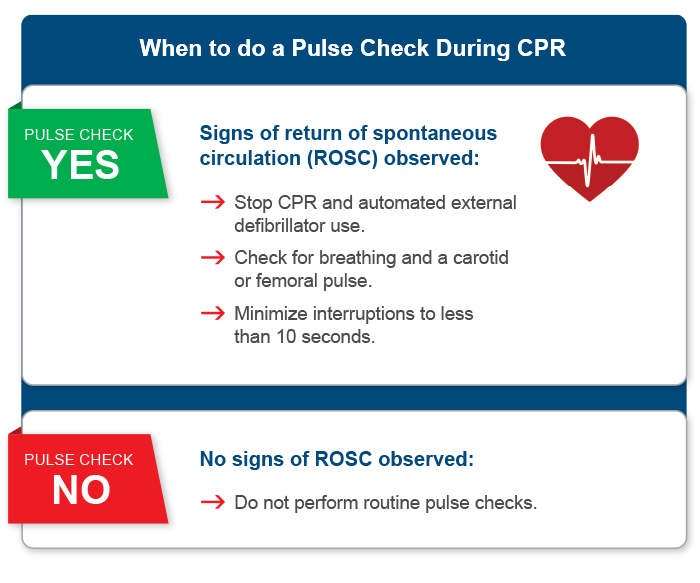
Insights and Implications
The value of a pulse check while CPR is in progress is uncertain, particularly in light of the difficulty in detecting a pulse despite training. Additionally, checking for a pulse during CPR has the potential to prolong pauses, leading to an associated reduction in CCF. If there are clinical, hemodynamic or end-tidal capnography signs of ROSC, it is reasonable to consider a pulse check if trained to do so.
Rhythm Check Timing
Last Full Review: ILCOR 2019
Last Update: 2023
Prolonged pauses during cardiopulmonary resuscitation (CPR) have been shown to be associated with lower odds for survival from ventricular fibrillation. Should cardiac rhythm be analyzed immediately after defibrillation, or should there be immediate resumption of chest compressions with delayed check of the cardiac rhythm?
Red Cross Guidelines
- Immediately after a shock is delivered, cardiopulmonary resuscitation (CPR) should be resumed for 2 minutes before pausing compressions to conduct a rhythm check.
- Based on the clinical situation, performing rhythm analysis after defibrillation may be considered by healthcare professionals.
- After every 2 minutes of CPR, the rhythm should be reassessed (while minimizing interruptions to CPR).
- If there are physiologic signs of return of spontaneous circulation, briefly pausing compressions for rhythm analysis may be considered.
Evidence Summary
A 2019 International Liaison Committee on Resuscitation (ILCOR) systematic review and Consensus on Science with Treatment Recommendations (Olasveengen et al. 2020, s41) evaluated a cardiac rhythm check immediately after defibrillation compared with the immediate resumption of chest compressions after defibrillation in adults with in-hospital cardiac arrest or out-of-hospital cardiac arrest and receiving a defibrillation attempt during CPR. Evidence included was of low or very low certainty due to risk of bias, indirectness or imprecision. None of the included studies were from the in-hospital or pediatric setting. The review (Olasveengen et al. 2020, s41) identified one randomized controlled trial (RCT) with 415 out-of-hospital cardiac arrests showing no improvement in survival with favorable neurologic outcome at discharge following interruption of chest compressions to check cardiac rhythm immediately after shock delivery (RR, 0.90; 95% CI, 0.7–1.15), (Beesems et al. 2016, 1) while three observational studies (Bobrow et al. 2008, 1158; Kellum, Kennedy and Ewy 2006, 335; Rea et al. 2006, 2760) of 763 out-of-hospital cardiac arrests showed an association between decreased survival with favorable neurologic outcome at discharge and interrupting chest compressions for a rhythm check immediately after defibrillation. Similar findings were reported for the outcome of survival to hospital admission. Two RCTs (Beesems et al. 2016, 1; Berdowski, Tijssen and Koster 2010, 72) with 551 out-of-hospital cardiac arrests did not show a reduction in the rate of recurrence of ventricular fibrillation with interruption of chest compressions to check cardiac rhythm immediately after defibrillation compared with the immediate resumption of compressions (RR, 1.08; 95% CI, 0.95–1.22) (Olasveengen et al. 2020, s41). A weak recommendation is made by ILCOR for the immediate resumption of chest compressions after shock delivery for adults in cardiac arrest in any setting (Olasveengen et al. 2020, s41). If there is alternative physiologic evidence of return of spontaneous circulation, chest compressions can be briefly paused for rhythm analysis (Olasveengen et al. 2020, s41).
Real-Time Feedback for CPR Quality
Last Full Review: ILCOR 2020
Last Update: 2024
Real-time cardiopulmonary resuscitation (CPR) feedback devices provide immediate feedback to the person performing CPR on a person in cardiac arrest. They are designed to help improve the quality and effectiveness of CPR by monitoring and providing real-time information about various aspects of the CPR being performed, such as chest compression depth, rate, recoil and in some cases—ventilation timing and adequacy. This feedback is intended to ultimately improve patient outcomes. Real-time audiovisual feedback and prompt devices have been recommended during CPR when used as part of a comprehensive quality improvement program (Olasveengen et al. 2020, S41).
Red Cross Guidelines
- Healthcare professionals may consider using feedback devices during real-time cardiopulmonary resuscitation (CPR) performance.
- Instructors may choose to incorporate feedback devices during CPR training to improve CPR performance.
Evidence Summary
A 2020 International Liaison Committee on Resuscitation (ILCOR) systematic review and Consensus on Science with Treatment Recommendations (Olasveengen et al. 2020, S41) of real-time CPR feedback devices was the subject of a scoping review in 2024 (Masterson et al. 2024, 100730; Masterson et al. 2024; Greif et al. 2024) with a new focus on additional interventions and their use in CPR by healthcare professionals responding in a professional capacity, rather than by bystanders or lay responders. The updated literature search identified further studies evaluating audiovisual feedback, such as metronome guidance for chest compression rate and feedback devices for compression depth, that suggest improved CPR quality when feedback devices are used. Only three studies reviewed included pediatric patients.
However, the studies reporting improved patient outcomes (other than return of spontaneous resuscitation) also included high-performance CPR, post-event debriefing and other interventions. The review concluded that the new evidence aligns with current ILCOR treatment recommendations. An update of the systematic review with the original Population Intervention Comparison Outcome Study Design Timeline (PICOST) question is planned, with subgroup analysis of feedback devices and separate reviews by provider type.
Insights and Implications
Cardiopulmonary resuscitation quality improvement programs typically use a variety of approaches, making the study of feedback devices in isolation from other interventions difficult. The Red Cross guidelines for the use of CPR feedback devices in real-time remain unchanged while awaiting an updated systematic review by ILCOR.
Bag-Mask Ventilation Versus Mouth-to-Mask Ventilation
Last Full Review: American Red Cross Scientific Advisory Council 2021
Are clinical outcomes improved when a lay responder/healthcare professional uses bag-mask ventilation (BMV) as compared with mouth-to-mask ventilation?
Red Cross Guidelines
-
A single person providing ventilations should use the mouth-to-mask technique rather than the bag-mask ventilation (BMV) technique.
- Multiple healthcare professionals may use the two-person BMV technique if properly trained and experienced in this method.
Evidence Summary
A 2021 updated scientific review by the American Red Cross Scientific Advisory Council sought evidence from January 2017 to January 2021 to support ventilation of a nonbreathing person with a BMV device compared with mouth-to-mask ventilation provided by a single person and when multiple trained lay responders or healthcare professionals are available. All clinical outcomes were considered. No studies met inclusion criteria, and guidelines remain unchanged. This topic was previously reviewed by the American Red Cross Scientific Advisory Council in 2017 and included one narrative review, six observational manikin studies and one observational cadaver study. The evidence that was included was of low to very low certainty and suggested an association between the use of mouth-to-mask ventilation and improved ventilations, less interruptions of chest compressions and improved skill retention at 1 year when compared with the use of BMV. Hyperventilation was less common with mouth-to-mask or mouth-to-face shield ventilation and was more common with BMV. The review concluded that mouth-to-pocket mask remains the best technique to teach lay responders ventilation of nonbreathing patients. Bag-mask ventilation is a more difficult skill to learn and retain.
Insights and Implications
Rescue breaths can be delivered by mouth-to-mouth (with or without a barrier device), or mouth-to-mask (with inline filter/one-way valve) while manual ventilations can be delivered with a bag-mask device. The mouth-to-mask technique appears easier to learn and remember than the BMV technique, has not been associated with any reported disease transmission, and allows for fewer interruptions in chest compressions than BMV technique by a single rescuer.
Tidal Volumes and Ventilation Rates
Last Full Review: ILCOR 2020 (Children and Infants); ILCOR 2010 (Adults)
Last Update: 2023 (Adults)
Guidelines for ventilation rates for children changed in 2020. For adults, guidelines for ventilation rates, tidal volumes and inspiratory rates have remained unchanged since 2010. Is there new science to suggest a need to reevaluate current guidelines?
Red Cross Guidelines
-
For adults with a pulse but insufficient respiratory effort, and during cardiopulmonary resuscitation (CPR) with an advanced airway in place, 1 rescue breath/manual ventilation should be provided every 6 seconds.
- For children and infants with a pulse but insufficient respiratory effort, and during CPR with an advanced airway in place, 1 rescue breath/manual ventilation should be provided every 2 to 3 seconds.
- Rescue breaths and manual ventilations should be delivered over 1 second in adults, children and infants and with a volume that produces visible initiation of chest rise.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council literature update did not identify new studies of inspiratory times, ventilation rates or tidal volumes for adults or children without advanced airways in place, and guidelines are unchanged. Historically, guidelines for the inspiratory time to deliver mouth-to-mouth and bag-mask ventilations in adults stem from a 2005 International Liaison Committee on Resuscitation (ILCOR) Consensus on Science with Treatment Recommendations, (International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Part 2 2005, 187) while guidelines for adult ventilatory rates and tidal volume reflect the treatment recommendations from a 2010 ILCOR review (Sayre et al. 2010, S298) of airway management.
The Red Cross guidelines for children and infants in respiratory arrest and cardiac arrest with an advanced airway in place changed in 2020 following publication of a large multicenter cohort study of ventilation in children receiving cardiopulmonary resuscitation (CPR) with an advanced airway in place (Sutton et al. 2019, 1627). The recommended ventilatory rate was changed to 1 breath or ventilation every 2 to 3 seconds. This change reflects:
-
A closer approximation with baseline physiologic pediatric respiratory rates.
-
The likelihood of an underlying respiratory process preceding a cardiac event in children.
- The findings from the 2019 multicenter cohort study that evaluated ventilation rates during CPR performed in children with an advanced airway, showing that higher ventilation rates (at least 30 breaths/minute in infants and 25 or more breaths/minute in older children) were associated with higher odds of return of spontaneous circulation and survival to hospital discharge (Sutton et al. 2019, 1627).
There are no recommendations by ILCOR regarding ventilation rates for children and infants with a perfusing rhythm and respiratory arrest (Maconochie et al. 2020, S140).
For adults, evidence supporting the guidelines for delivery of a rescue breath or manual ventilation over 1 second includes a secondary analysis of case series (Aufderheide and Lurie 2004, S345; Aufderheide et al. 2004, 1960) that included patients with advanced airways after out-of-hospital cardiac arrest. Ventilation rates above 10 per minute and inspiration times greater than 1 second were associated with no survival (International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Part 2 2005, 187). In addition, a 2005 study using a model of a simulated unprotected airway reported that a reduction of peak inspiratory time from 2 seconds to 1 second resulted in a significant increase in peak airway pressure and peak inspiratory flow rate, with no increase in stomach inflation (von Goedecke et al. 2005, 321).
Evidence supporting guidelines for ventilatory rates and tidal volume in adults includes human studies showing that oxygenation and normocarbia were maintained in apneic adults who were ventilated with room air and tidal volumes of 600 milliliters (ml), while supplemental oxygen was needed to reach adequate saturation levels when tidal volumes of 500 ml were used (Sayre et al. 2010, S298).
Αn evidence update (Berg et al., 2023) by ILCOR in 2022 did not identify new relevant studies of tidal volume or ventilation rate. Of note, neonatal and infant studies were excluded from the literature update search, as were studies involving patients who were intubated.
Insights and Implications
Excessive ventilation (rate and volume) can cause gastric insufflation with regurgitation and aspiration, increased intrathoracic pressure, and decreased cardiac venous return and output, and should be avoided. For patients with an advanced airway in place during CPR, the reduced cardiac output should support a lower minute ventilation and tidal volume of about 500 ml to 600 ml (6 ml/kg to 7 ml/kilogram [kg]). For patients without an advanced airway in place, this volume equates to seeing the initiation of chest rise. Delivering ventilations over 1 second instead of 2 also allows for higher chest compression rates without increased risk of gastric insufflation.
The Red Cross guidelines for ventilation rates in children and infants with a pulse but with respiratory insufficiency are based largely on indirect evidence from the 2019 multicenter cohort study (Sutton et al., 2019, 1627) showing that among intubated patients, higher ventilation rates (at least 30 breaths/minute in infants and 25 or more breaths/minute in older children) were associated with higher odds of return of spontaneous circulation and survival to hospital discharge.
CPR Compression-to-Ventilation Ratios for Adults
Last Full Review: ILCOR 2025
The use of standard, compression-ventilation cardiopulmonary resuscitation (CV-CPR) is recommended for adults and children in cardiac arrest without an advanced airway. For adults, the compression-to-ventilation ratio changed in 2005 from 15:2 to a 30:2 ratio. A full systematic review by the International Liaison Committee on Resuscitation (ILCOR) in 2017 supported recommendations for the 30:2 compression-ventilation ratio in adults but was based on studies performed during the transition period between ratios. This topic was the subject of an updated systematic review for 2025.
Red Cross Guidelines
- Standard cardiopulmonary resuscitation with a compression-to-ventilation ratio of 30:2 should be used for adults in cardiac arrest without an advanced airway.
- With an advanced airway in place, healthcare and prehospital professionals should not pause compressions for ventilations.
Evidence Summary
An updated ILCOR systematic review and Consensus on Science with Treatment Recommendations (CoSTR) sought evidence for the use of any CPR ratio delivered by emergency medical services (EMS) compared with an alternative ratio (Nehme et al. 2024a; Bray et al. 2025, S34). Clinical outcomes of interest included favorable neurological survival, survival to discharge, survival to 30 days or any time interval after discharge, and return of spontaneous circulation. All included studies were conducted before 2012 and evaluated the impact of the 2005 resuscitation guideline changes, including a change in the compression-to-ventilation ratio from 15:2 to 30:2 for adults. No studies specifically looked at compression-to-ventilation ratios in the pediatric population. For the comparison of a 30:2 ratio versus 15:2, two studies of out-of-hospital cardiac arrest (OHCA) from all rhythms showed an improved risk adjusted odds of survival with a 30:2 ratio (Sayre et al. 2009, 469; Steinmetz et al. 2008, 908), while one study did not (Olasveengen et al. 2009, 407). One study of OHCA with an initial nonshockable rhythm showed an increased risk adjusted odds of survival and survival to 12 months with a 30:2 ratio compared to 15:2 (Kudenchuk et al. 2012, 1787). One study (Garza et al. 2009, 2597) reported improved survival to discharge following bystander witnessed OHCA with a compression-to-ventilation ratio of 50:2 compared to 5:1.
The ILCOR treatment recommendation remains unchanged, with a weak recommendation that suggests a compression-to-ventilation ratio of 30:2 compared with any other compression-to-ventilation ratio in adult patients in cardiac arrest (Nehme et al. 2024a; Bray et al. 2025, S34).
Insights and Implications
It should be noted that this ILCOR review does not address compression-to-ventilation ratios when an advanced airway is in place, and while the review question focused on compression-to-ventilation ratios in CPR delivered by EMS, the ILCOR treatment recommendations do not specify that the recommendation is targeted at any type or level of provider or in-hospital versus out-of-hospital settings. The Red Cross CPR training includes the delivery of ventilations with compressions, and thus, the ILCOR review and recommendations are used to inform guidelines for standard CPR with compressions and ventilations for EMS healthcare professionals and others trained in standard compression-ventilation CPR.
The studies included in this systematic review were all performed at a time when guidelines changed from a 15:2 ratio to a 30:2 ratio as part of a bundle of care that included other changes, such as an increase in CPR duration cycles, removal of post-shock rhythm checks and efforts to reduce interruptions to chest compressions. This makes it difficult to determine if the benefits reported in the studies are related to other changes made in CPR techniques. The ILCOR review noted one study (Rea et al. 2006, 2760) that reported improved survival to hospital discharge with bystander-witnessed OHCA and an initial shockable rhythm after a change in guidelines that did not include adopting the 30:2 compression-to-ventilation ratio recommendation. More studies are needed, particularly those looking at longer compression-to-ventilation ratios compared to 30:2.
CPR Compression-to-Ventilation Ratio for Children and Infants: Healthcare Professionals
Last Full Review: ILCOR 2017
Last Update: 2022
Since 2015, it has been recommended by the Red Cross that lay responders and healthcare professionals provide rescue breaths and chest compressions for children and infants with in-hospital cardiac arrest and out-of-hospital cardiac arrest. It has also been a Red Cross guideline recommendation that if someone is unwilling or unable to provide ventilations (i.e., mouth-to-mouth, mouth-to-mask) for children and infants in cardiac arrest, they should at least perform chest compressions. Is there new evidence to support these recommendations?
Red Cross Guidelines
- For children and infants, a compression-to-ventilation ratio of 30:2 should be used by one healthcare professional and a ratio of 15:2 should be used by two healthcare professionals, while a ratio of 30:2 should be used by a lay responder.
- For children and infants with an advanced airway in place, healthcare professionals should deliver 1 ventilation every 2 to 3 seconds (20 to 30 breaths per minute) with continuous compressions.
- Compression-only cardiopulmonary resuscitation (CPR) may be used as an alternative to CPR with compressions and ventilations when someone is unwilling or unable to provide ventilations.
Evidence Summary
An evidence update (Wyckoff et al. 2022,e483) of a 2017 International Liaison Committee on Resuscitation (ILCOR) Consensus on Science with Treatment Recommendations (Olasveengen et al. 2017, e424) on compression-only cardiopulmonary resuscitation (CO-CPR) in pediatric patients identified one relevant study. A retrospective review of data from the Cardiac Arrest Registry to Enhance Survival database evaluated 13,060 pediatric (18 years of age or younger) nontraumatic out-of-hospital cardiac arrests (Naim et al. 2021,1042). In multivariable analysis of the overall cohort, neurologically favorable survival was associated with rescue-breathing cardiopulmonary resuscitation (aOR, 2.16; 95% CI, 1.78–2.62) and with CO-CPR (aOR, 1.61; 95% CI, 1.34–1.94) compared with no CPR. Rescue-breathing CPR was associated with higher odds of neurologically favorable survival compared with CO-CPR (aOR, 1.36; 95% CI, 1.10–1.68). Risk stratification by age group was also reported. For the comparison of RB-CPR with no CPR, adjusted odd ratio for neurologically favorable survival was greater for infants less than 1 year old (aOR, 1.65; 95% CI, 1.19–2.3; P<0.003), children (1 to 11 years of age) (aOR, 2.73; 95% CI, 2.00–3.72; P<0.001) and adolescents (12 years of age or older) (aOR 2.12; 95% CI, 1.44–3.11; P<0.001). When comparing data for patients who received CO-CPR with data for patients with no CPR, CO-CPR was associated with better neurologically favorable survival in children (aOR 1.94; 95% CI, 1.41–2.68; P<0.001) and adolescents (aOR, 1.71; 95% CI, 1.23–2.37; P<0.001), but not for infants (aOR, 1.16; 95% CI, 0.083–1.62; P=0.294) (Naim et al. 2021,1042). The identified study was considered supportive of current ILCOR recommendations for providing rescue breathing with chest compressions in pediatric in-hospital cardiac arrest and out-of-hospital cardiac arrest and for providing CO-CPR when rescuers are unwilling or unable to provide rescue breathing. The evidence update authors noted that a previously identified study from 2010 (Kitamura et al. 2010,1347) found that CO-CPR for infants was not associated with a more favorable neurologic outcome compared with no CPR. Although the new study (Naim et al. 2021,1042) also found that CO-CPR was not associated with better neurologically favorable survival for infants compared with no CPR, the ILCOR Pediatric Task Force continues to recommend CO-CPR for infants in cardiac arrest when rescuers are unwilling or unable to provide rescue breathing (Wyckoff et al. 2022, e483).
Insights and Implications
The Red Cross guidelines for the use of compression-ventilation CPR in children and infants and for the use of CO-CPR when someone is unwilling or unable to provide ventilations are reaffirmed with this ILCOR evidence update. Further studies are needed to determine the benefit of CO-CPR for infants.
Bystander Compression-Only CPR (Without Dispatcher-Assisted CPR) Versus Conventional CPR in Adults
Last Full Review: ILCOR 2025
Last Update: 2022
Bystander cardiopulmonary resuscitation (CPR) has been shown to more than double survival from out-of-hospital cardiac arrest (OHCA). The introduction of compression-only CPR (CO-CPR) has been shown to increase rates of bystander CPR (Bray et al. 2011, 1393; Iwami et al. 2015, 415; Malta Hansen et al. 2015, 255; Kitamura et al. 2012, 2834), and surveys show that compression-only CPR is preferred by bystanders when a stranger needs CPR (Cheskes et al. 2016, 253; Bray et al. 2017, 158). Red Cross Basic Life Support CPR teaches standard compression-ventilation CPR (CV-CPR), with CO-CPR advised for those who are untrained or unwilling to provide ventilations. An updated systematic review by the International Liaison Committee on Resuscitation (ILCOR) looked at clinical outcomes in adults in cardiac arrest who received CO-CPR by bystanders, compared with CV-CPR.
Red Cross Guidelines
- Chest compressions should be provided for all adults in cardiac arrest. (Good practice statement)
- For bystanders who are trained, able and willing, chest compressions with rescue breaths or ventilations are suggested for adults in cardiac arrest.
Evidence Summary
A 2025 ILCOR systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Bray et al. 2025 ILCOR; Bray et al. 2025, S34) evaluated evidence from studies looking at the use of chest compression-only CPR (CO-CPR) compared with conventional CPR (CV-CPR) using compressions and ventilations on adults with OHCA. This was an update of a 2017 ILCOR systematic review (Ashoor et al. 2017, 112) with a revised search strategy and a review plan that excluded observational studies not reporting adjusted outcomes (due to imbalances between groups known to influence survival). In addition, to look explicitly at the provision of immediate bystander CPR, studies in which bystander CPR was assisted by dispatchers were excluded. Three observational studies were ultimately included, with two studies comparing bystander CO-CPR with conventional CPR at a ratio of 15 compressions to 2 ventilations (15:2) (Bohm et al. 2007, 2908; Ong et al. 2008, 119), while the third study used a CV-CPR ratio of 30 compressions to 2 ventilations (30:2) (Bobrow et al. 2010, 1447). However, if no data was available for a selected outcome, indirect evidence from combined bystander compression-only CPR and dispatcher-assisted CPR studies was presented if the sample included high rates of bystander compressions-only CPR.
Results from one cohort study with combined data from bystander CPR cases (SOS-KANTO 2007, 920) and dispatcher-assisted CPR cases (24 percent) suggested favorable neurological function with CO-CPR compared to standard CV-CPR with a 15:2 ratio in witnessed adult OHCA (SOS-KANTO 2007, 920). Of the observational studies focused on bystander CPR without dispatcher assistance, Bobrow et al. (Bobrow et al. 2010, 1447) reported higher survival to hospital discharge with CO-CPR compared to 30:2 standard CV-CPR, while no difference was found in the other two studies for survival to 30 days and 15:2 CPR (Bohm et al. 2007, 2908) or survival to hospital discharge (Ong et al. 2008, 119). Other outcomes in which a difference was not found between CO-CPR and 15:2 CV-CPR included survival to hospital admission (Bohm et al. 2007, 2908) and return of spontaneous circulation (Ong et al. 2008, 119).
The ILCOR treatment recommendations include a good practice statement that chest compressions be performed for all adults in cardiac arrest, and a weak recommendation suggesting that bystanders who are trained, able and willing give chest compressions with rescue breaths for adults in cardiac arrest (Bray et al. 2024; Bray et al. 2025, S34).
Insights and Implications
The “weak” recommendation by ILCOR for giving chest compressions with rescue breaths for adults in cardiac arrest reflects the very low-certainty evidence and comparison to 15:2 CV-CPR ratios. There is a general lack of studies comparing CO-CPR to 30:2 CV-CPR without dispatcher assistance. The ILCOR review noted that other studies not included in the evidence review that used unadjusted data also reported no significant difference in patient outcomes between CO-CPR and CV-CPR. Two adult studies that included dispatcher-assisted CPR (Fukuda et al. 2017, 493; Javaudin et al. 2021, 812) also found no difference in good neurological outcomes between bystander CO-CPR and CV-CPR in OHCA with respiratory or asphyxial etiologies. Most recently, a pilot randomized controlled trial that included dispatcher-assisted CPR did not show a difference in survival at 1 day for CO-CPR versus CV-CPR provided by trained laypersons (Riva et al. 2024, e10027).
The Red Cross guidelines have been updated based on the ILCOR review to first recommend that all adults in cardiac arrest receive chest compressions. The recommendation to provide CPR with ventilations has been reworded for clarity but remains consistent with previous recommendations to provide CPR with ventilations if trained, able and willing.
.
Fatigue with Chest-Compression-Only CPR
Last Full Review: ILCOR 2020
Last Update: 2022
Red Cross guidelines allow for providing compression-only cardiopulmonary resuscitation (CO-CPR) as an alternative to conventional compression-ventilation CPR (CV-CPR) when a rescuer is unwilling or unable to provide ventilations. Does providing CO-CPR to adult or pediatric patients in cardiac arrest compared with CV-CPR increase rescuer fatigue with a subsequent decrease in the quality of chest compressions?
Red Cross Guidelines
- Compression-only cardiopulmonary resuscitation (CPR) may be used as an alternative to CPR with compressions and ventilations when someone is unwilling or unable to provide ventilations.
- Compression-only CPR should be continued unless it is no longer possible due to physical exhaustion.
Evidence Summary
A 2022 evidence update by the International Liaison Committee on Resuscitation identified simulation studies with manikins investigating resting frequency during CO-CPR (Wyckoff et al. 2022, e483). Results of these studies were not felt to warrant a change in guidelines, but it was suggested that subsequent to the coronavirus disease 2019 pandemic and increase in CO-CPR, future studies evaluating rest duration and frequency during CO-CPR should be considered. The International Liaison Committee on Resuscitation currently recommends that no modification be made to current CO-CPR guidelines for cardiac arrest to mitigate rescuer fatigue.
Insights and Implications
The relationship between rescuer fatigue during CO-CPR and chest compression quality continues to be a knowledge gap in need of future research. The Red Cross guideline for continuing CO-CPR unless it is no longer possible due to physical exhaustion is in addition to the standing guidance to continue CPR/automated external defibrillator until:
- The team leader tells you to stop.
- Other trained healthcare professionals arrive and relieve you.
- There are signs of life/return of spontaneous circulation.
- You are presented with a valid do not resuscitate order.
- The situation becomes unsafe to continue.
Impact of Wearing Personal Protective Equipment on Quality of CPR
Last Full Review: ILCOR 2023
Providing high-quality cardiopulmonary resuscitation (CPR) leads to rescuer fatigue, particularly with compression-only CPR, and has led to past recommendations to rotate compressors every 2 minutes. Since the advent of coronavirus disease 2019, more personal protective equipment (PPE) is being worn by healthcare professionals and lay responders. This has raised questions about the effect of wearing PPE on the quality of CPR and clinical outcomes.
Red Cross Guidelines
- During cardiopulmonary resuscitation (CPR), the team leader should monitor team members providing CPR for signs of fatigue.
- Team members should switch off giving compressions every 2 minutes, or sooner as the team member giving compressions may be fatigued.
Evidence Summary
A 2023 systematic review (Chung et al. 2023, 100398) and Consensus on Science with Treatment Recommendations (Chung et al. 2023) by the International Liaison Committee on Resuscitation (ILCOR) sought to determine the impact of wearing PPE during CPR on the quality of CPR and patient outcomes. The review included 10 studies of simulated cardiac arrest and one clinical study (Ko et al. 2021, 1291). No difference in 30-day survival was reported in the clinical study with enhanced PPE use compared with conventional PPE use (adjusted multivariate logistic analysis [aOR], 0.38; 95% CI, 0.07–2.10; P=0.27), and no difference in return of spontaneous circulation was reported when using enhanced PPE (aOR, 0.79; 95% CI, 0.38–1.67; P=0.54) (Ko et al. 2021, 1291). Conventional PPE in this study included a surgical mask, gloves and a gown. Enhanced PPE included a complete bodysuit, boots, an N95 respirator and a powered air-purifying respirator.
Meta-analyses of randomized controlled trials and observational studies using manikins also reported no difference in CPR quality as measured by chest compression rate, depth and hands-off time between rescuers wearing PPE compared with no PPE (Chung et al. 2023, 100398). Pooled subjective rescuer fatigue from six studies, as reported by visual analogue score, was greater in the group wearing PPE compared with not wearing PPE. The review concludes that while rescuers wearing PPE may report more fatigue while performing CPR on manikins, wearing PPE was not associated with reduced CPR quality. The single clinical study (Ko et al. 2021, 1291) did not find a difference in survival when comparing the use of enhanced PPE with conventional PPE, but additional studies are needed (Chung et al. 2023; Chung et al. 2023, 100398).
The ILCOR treatment recommendations stemming from this review include a good practice statement that recommends monitoring for fatigue in all rescuers performing CPR. Because rescuers wearing PPE may have greater fatigue, increased vigilance for fatigue is suggested in these circumstances (Chung et al. 2023, 100398; Chung et al. 2023).
Insights and Implications
Although wearing PPE was not shown in the simulation studies to impact CPR quality, additional studies are needed in clinical scenarios and with patient outcomes. Rotating team members who are providing chest compressions every 2 minutes or less is one means to reduce the impact of fatigue on CPR quality. Monitoring for fatigue in all rescuers performing CPR is recommended as an ILCOR good practice statement (Chung et al. 2023, 14; Chung et al. 2023). Team members may not recognize their own fatigue. A manikin study reported a significant decline in chest compressions reaching the recommended depth between the first and fifth minutes of CPR, while chest compression rate and rescue breath volume were unaffected (McDonald et al. 2013, 623). Other studies have shown a decrease in the quality of CPR as measured by the depth of chest compressions and the number of adequate chest compressions per minute, with a higher number of adequate chest compressions reported with conventional CPR compared with compression-only CPR (Shin et al. 2014, 59).
CPR Quality During Transport
Last Full Review: ILCOR 2022; American Red Cross Scientific Advisory Council 2015
Prehospital healthcare professionals responding to out-of-hospital cardiac arrests are sometimes faced with the decision to either continue cardiopulmonary resuscitation (CPR) on-scene or to transport a patient to the hospital while continuing to provide CPR. Often, the decision is based on predetermined emergency medical services (EMS) transport criteria or termination of resuscitation rules. Is there evidence to support one approach versus another?
Red Cross Guidelines
- The decision to transport a patient following out-of-hospital cardiac arrest and while cardiopulmonary resuscitation (CPR) is in progress should be made based on emergency medical services protocols and/or in consultation with on-line medical control.
- Protocols to determine care on-scene versus during transport for out-of-hospital cardiac arrest should be evidence-based, and at a minimum, consider local resources, competency of providers and distances to hospital care.
- There should be separate protocols for adults and for infants and children.
- When transporting an out-of-hospital cardiac arrest care patient to a hospital, prehospital healthcare professionals should strive to deliver high-quality CPR.
Evidence Summary
A 2022 systematic review and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2022, e483; Smyth et al. 2022) by the International Liaison Committee on Resuscitation (ILCOR) looked at the effect of transporting a patient following out-of-hospital cardiac arrest with ongoing CPR compared with completing CPR on the scene. Outcomes of interest included survival to hospital discharge, favorable neurological outcome, return of spontaneous circulation (ROSC), and quality of CPR metrics on-scene versus during transport. No studies were identified evaluating the effect that CPR quality during transport had on patient outcomes. Both manikin studies and observational studies were included for evaluation of CPR quality metrics. Findings reported from the limited number of observational studies of CPR metrics during transport were varied, with some reporting no differences in chest compression rate and depth, CPR fraction or ventilation rate, while some studies reported negative impacts on these metrics. Most studies reported a lower CPR fraction during transport. A single observational study enrolling 27,705 patients reported on the impact of transport while providing CPR on ROSC, survival to hospital discharge and hospital discharge with favorable neurologic outcome (Grunau et al. 2020, 1058). Fewer patients in the CPR during transport group were discharged with favorable neurologic outcome (RR, 0.39; 95% CI, 0.33–0.47; 2 patients fewer/1,000 [2 fewer to 3 fewer]), fewer survived to hospital discharge (RR, 0.46; 95% CI, 0.42–0.52; 5 patients fewer/1,000 [4 fewer to 5 fewer]), and fewer achieved ROSC (RR, 0.41; 95% CI, 0.39–0.43; 23 patients fewer/1,000 [22 fewer to 24 fewer]). Evidence was judged as very low certainty (Wyckoff et al. 2022, e483; Smyth et al. 2022). A weak recommendation was made by ILCOR suggesting that providers deliver resuscitation at the scene rather than undertake ambulance transport with ongoing resuscitation unless there is an appropriate indication to justify transport. A strong recommendation was made that whenever transport is indicated, EMS providers should focus on the delivery of high-quality CPR throughout transport (Wyckoff et al. 2022, e483; Smyth et al. 2022).
Insights and Implications
Providing CPR in a moving vehicle can be challenging and thus findings for the CPR metric outcomes are not unexpected. Data for survival, survival with favorable neurologic outcome, and ROSC, however, are from a single study with very low-certainty evidence and therefore more difficult to interpret. The decision to transport and when or where to transport is complex and in some cases, multifactorial. Emergency medical services protocols should be followed, where available, and when questions arise, EMS Medical Command should be contacted for advice.
Passive Ventilation Techniques During CPR
Last Full Review: ILCOR 2022
Passive ventilation or oxygen insufflation during resuscitation from out-of-hospital cardiac arrest offers an alternative to positive pressure ventilations (PPVs) and oxygen delivery. Initial passive ventilation has been reported to be associated with higher neurologically intact survival to hospital discharge when compared with initial bag-mask ventilation in emergency medical services (EMS) systems when combined with minimally interrupted cardiac resuscitation (Bobrow et al. 2009, 656).
Red Cross Guidelines
- There is insufficient evidence to support the routine use of passive ventilation techniques during conventional cardiopulmonary resuscitation.
- The use of passive ventilation techniques may be considered by prehospital healthcare professionals as part of a bundle of care to include minimally interrupted cardiac resuscitation.
Evidence Summary
A 2022 International Liaison Committee on Resuscitation (ILCOR) systematic review and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2022, e483; Ristagno et al. 2022) evaluated the use of any passive ventilation technique in addition to chest compressions, compared with conventional compression-ventilation cardiopulmonary resuscitation (CV-CPR) in adults and children with presumed cardiac arrest in any setting. Very low-certainty evidence from two randomized controlled trials (RCTs), an observational study and a small pilot RCT were identified (Bobrow et al. 2009, 656; Saïssy et al. 2000, 1523; Bertrand et al. 2006, 843; Fuest et al. 2021, 85). The two RCTs used intermittent PPV through a tracheal tube compared with continuous insufflation of oxygen using a modified (Boussignac) tracheal tube; an active compression-decompression device was used for chest compressions when available and may have contributed to passive ventilation. Results from the observational study (Bobrow et al. 2009, 656) were considered difficult to interpret due to confounding from differing CPR protocols (Wyckoff et al. 2022, e483; Ristagno et al. 2022). Overall, no benefit from passive ventilation was found for outcomes of survival to intensive care unit discharge, survival to hospital admission and return of spontaneous circulation. The ILCOR treatment recommendation suggests against the routine use of passive ventilation techniques during conventional CPR (Wyckoff et al. 2022, e483; Ristagno et al. 2022).
Insights and Implications
Passive ventilation techniques during chest compressions can be used with or without oxygen and include positioning of the body, opening the airway and using airway adjuncts, use of a passive oxygen administration and constant flow insufflation. Some EMS systems provide continuous chest compressions with passive ventilation using an oropharyngeal airway and oxygen delivery through a simple face mask. Whether chest compressions generate a sufficient tidal volume for gas exchange is uncertain and may vary with the duration of resuscitation. Despite the lack of evidence to support passive ventilation in the ILCOR review, a strategy by EMS systems that includes minimally interrupted CPR with passive ventilation is considered reasonable.
Ventilations for Patients with Respiratory Insufficiency or an Advanced Airway
Last Full Review: ILCOR 2019
Last Update: 2021
The rate at which ventilations are provided in the absence of sufficient respiratory effort but with perfusion and during cardiopulmonary resuscitation (CPR) has been discussed in prior guidelines. There has also been debate about whether there should be a universal approach or whether there should be alterations for children and infants. Lastly, the use of bag-mask ventilation and pocket masks have been a source of prior debate.
Red Cross Guidelines
- For adults, 1 ventilation should be provided every 6 seconds for a person with a pulse but insufficient respiratory effort, and during cardiopulmonary resuscitation (CPR) with an advanced airway in place.
- For children and infants, 1 ventilation should be provided every 2 to 3 seconds for a child or infant with a pulse but insufficient respiratory effort, and during CPR with an advanced airway in place.
- Bag-mask ventilation (BMV) should be performed as a two-person technique.
- When there is only one healthcare professional to provide ventilation, a pocket mask should be preferred over BMV.
Evidence Summary
The ventilation rate and providing ventilations with an advanced airway have been the subject of prior International Liaison Committee on Resuscitation (ILCOR) and American Red Cross Scientific Advisory Council evaluations. There have been no recent reviews by the American Red Cross Scientific Advisory Council or ILCOR with regard to adult ventilation rates and providing ventilation with an advanced airway. For pediatric ventilation rates, the rate has changed over the years in subsequent guidelines issues. A recently published multicenter cohort study (Sutton et al. 2019, 1627) evaluated ventilation rates in 52 events requiring at least 1 minute of CPR in 47 intubated children, finding that higher ventilation rates (at least 30 breaths/minute in children under 1 year of age and 25 or more breaths/minute in older children) were associated with higher odds of return of spontaneous circulation and survival to discharge. The use of pocket mask versus bag-mask ventilation have been the subject of prior American Red Cross Scientific Advisory Council reviews and no new evidence was found to change these recommendations.
Insights and Implications
This single study was weighed by the American Red Cross Scientific Advisory Council against the benefit of education of single ventilation rate for all resuscitation. Findings from the specific study population of intubated children in a pediatric intensive care unit may not be generalizable. However, children have a higher baseline respiratory rate and cardiac arrests are more commonly triggered by respiratory issues than for adults. Additionally, because cardiac arrests are so rare in children, it will be difficult to replicate this study. For these reasons, a new recommendation is made by American Red Cross Scientific Advisory Council to provide increased ventilation rates for children and infants in respiratory arrest and in cardiac arrest with an advanced airway in place.
Alternative Cardiac Resuscitation Techniques
Last Full Review: ILCOR 2020
Last Update: 2023
Alternative techniques have been described for converting a malignant cardiac rhythm or for maintaining cardiac output to support consciousness. These include the use of a precordial thump for ventricular tachycardia (VT), “cough cardiopulmonary resuscitation (CPR)” (in conscious patients) for ventricular fibrillation, asystole or high-grade atrioventricular block, and percussion pacing (“fist pacing”) for asystole or bradycardia. Is there evidence to support the use of these alternative techniques?
Red Cross Guidelines
-
A precordial thump and percussion pacing should not be used for cardiac arrest.
- “Cough cardiopulmonary resuscitation” should not be used for cardiac arrest.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council literature update did not identify new human studies related to “cough CPR,” precordial thumps, and percussion (“fist”) pacing for adults in cardiac arrest, and guidelines remain unchanged. A 2020 International Liaison Committee on Resuscitation Consensus on Science with Treatment Recommendations (Olasveengen et al. 2020, S41) and accompanying systematic review (Dee et al. 2021, 73) evaluated the use of cough CPR, precordial thumps and percussion pacing on clinical outcomes following cardiac arrest. The evidence evaluated in this review suggests that there is no association between the use of a precordial thump and survival to hospital discharge. Evidence was not identified showing improved clinical outcomes following cardiac arrest with the use of either cough CPR or percussion pacing (Dee et al. 2021, 73).
Insights and Implications
Studies of cough CPR are limited to a small cohort study of in-hospital patients with VT and case series from the cardiac catheterization laboratory and the coronary care unit. The evidence for percussion pacing was limited to case series. While there may be exceptional circumstances where these techniques are considered, such as for a witnessed in-hospital cardiac arrest in a monitored setting or catheterization laboratory, the Red Cross does not recommend their use for cardiac arrest.
Harm to Those Performing CPR
Last Full Review: American Red Cross Scientific Advisory Council 2021; ILCOR 2020
Last Update: 2023
Harm related to the provision of cardiopulmonary resuscitation (CPR) is uncommon and may be physical (injury or illness) or emotional. The coronavirus disease 2019 (COVID-19) pandemic has led to renewed interest in the risks of harm to oneself associated with performing CPR, particularly the potential for transmission of infectious disease. What evidence exists demonstrating harm to lay responders or healthcare professionals because of performing CPR?
Red Cross Guidelines
- Although the risk of harm while performing cardiopulmonary resuscitation (CPR) is considered low, precautions should be taken to minimize the risk of transmission of infectious disease or defibrillator-associated injury. This may include, but is not limited to:
- Using standard precautions to provide patient care in all settings, to include performance of hand hygiene and use of personal protective equipment (PPE) (i.e., gloves, gown and a face mask) based on activities being performed and the risk assessment.
- Using additional PPE, including an N95 or higher-level respirator, and eye protection (goggles or face shield) for aerosol-generating procedures or resuscitation of patients. Disposable N95 respirators should be discarded after leaving the patient’s room or care area.
- Using an inline filter for mouth-to-mask or bag-mask ventilation.
- Performing hand hygiene after removal and disposal of PPE or after providing CPR without PPE.
- Avoiding touching a person in cardiac arrest when advised by automated external defibrillator prompts prior to the delivery of a shock.
Evidence Summary
A 2021 American Red Cross Scientific Advisory Council scientific review (American Red Cross Scientific Advisory Council: First Aid 2021a) evaluated the risk of infection during CPR and first aid, while an American Red Cross Scientific Advisory Council literature update sought studies describing other forms of harm to individuals providing CPR.
The American Red Cross Scientific Advisory Council Review and literature update identified one systematic review (Couper et al. 2020, 59) (updated in 2021) (Wyckoff et al. 2022, e645; Wyckoff et al. 2021, 229) evaluating the risk of COVID-19 transmission to rescuers performing chest compressions, defibrillation and CPR. Of the included cohort studies, case-control studies, case reports and manikin randomized controlled trials, 2 case reports and a cadaver study reported generation of aerosols during delivery of chest compressions, defibrillation or CPR. It was concluded that chest compressions and CPR have the potential to generate aerosols, and suggested that in the current COVID-19 pandemic, healthcare professionals use personal protective equipment (PPE) or aerosol-generating procedures during resuscitation, although it is reasonable to consider defibrillation before donning PPE in situations where the benefits may exceed the risks. For children in need of CPR, it is suggested that lay responders who are willing, trained and able, consider providing rescue breaths in addition to chest compressions (Wyckoff et al. 2022, e645; Wyckoff et al. 2021, 229; Couper et al. 2020, 59).
The 2021 American Red Cross Scientific Advisory Council scientific review (Couper et al. 2020, 59) evaluated the risk of transmission of infectious disease (not solely coronavirus). Eight case reports identified in this review document transmission of a variety of infectious disease during resuscitation. In most cases, PPE in the form of gloves or a barrier device for rescue breathing were not used. In one retrospective cohort study, (Ran et al. 2020, 2218) 72 healthcare workers with respiratory symptoms were followed for diagnosis of COVID-19. Thirty-three of these workers were classified as high risk based on their job location and 39 persons were classified as general risk based on their job location. The high-risk group had a 2.13 relative risk of developing COVID-19 compared with the general risk group. Suboptimal hand hygiene and improper PPE (undefined) were associated with an increased risk of contracting COVID-19 (RR, 3.10; 95% CI, 1.43–6.73; and RR, 2.43; 95% CI, 1.34–4.39, respectively). One case-control study (Liu et al. 2009, 52) evaluated 51 severe acute respiratory syndrome (SARS)-infected healthcare workers (compared with 426 uninfected controls) who had self-reported exposure to SARS patients and reported that chest compressions were significantly associated with high risk for infection (OR, 4.52; 95% CI, 1.08–18.81; P=0.031). However, in multivariate analysis it was not possible to distinguish between chest compressions and intubation. Wearing protective goggles, gloves and protective gowns were all found to reduce the risk of infection (P values 0.046, 0.011, 0.052, respectively; raw data not provided). Not wearing a mask was found to be a risk for contracting SARS (P=0.002).
A search of the grey literature identified an investigative report (News TGaKH 2020) by The Guardian and Kaiser Health News documenting 3,607 United States healthcare worker deaths from COVID-19 between March 2020 and April 2021, of which 7 percent were medical first responders. A subset of 654 first responder cases documented if there were concerns expressed (by patient, family or colleagues) about having adequate amounts of PPE available. Within this subset, 145 cases had concerns about having adequate amounts of PPE, 165 did not have concerns and, in 344, it was unknown.
Harm to rescuers from CPR was last reviewed systematically by the International Liaison Committee on Resuscitation in 2010, (Mancini et al. 2010, S539) followed by a scoping review in 2020 (Olasveengen et al. 2020, S41). The original 2010 ILCOR systematic review (Mancini et al. 2010, S539) was a multifaceted evaluation of the evidence for the safety of rescuers during training and clinical CPR performance and while using defibrillators, and for the impact of barrier device use on reducing infectious disease transmission. Evidence was sought for adverse physical effects, including injuries or fatigue, psychological effects and for infectious disease transmission. Treatment recommendations stemming from this review included consideration of changing rescuers after about 2 minutes of CPR to prevent rescuer fatigue, while minimizing interruptions to compressions, and pausing compressions during delivery of a shock. It was deemed reasonable to wear PPE while performing CPR. Although evidence was limited, the provision of CPR was felt to be safe for rescuers, with few reports of disease transmission or injury (Mancini et al. 2010, S539).
The 2020 ILCOR scoping review (Olasveengen et al. 2020, S41) of this topic identified several additional experimental studies and a case report. The identified studies primarily evaluated the safety of hands-on defibrillation while using gloves during chest compression. This review also noted that evidence supporting rescuer safety during CPR is limited, with few reports of possible disease transmission following mouth-to-mouth resuscitation, and a low incidence of defibrillator-related injuries to rescuers. The overall body of evidence was felt insufficient to warrant a full systematic review (Olasveengen et al. 2020, S41).
Insights and Implications
In general, the provision of CPR is considered low risk to providers. Physical injuries, such as back or muscle strain, may occur, and fatigue is common. There are relatively few reports of infectious disease transmission following provision of CPR. Despite the lack of direct evidence showing an association between chest compressions or defibrillation and transmission of COVID-19 to rescuers, lay responders and healthcare professionals can proactively reduce any risk through the use of PPE, when available, including the use of face masks, eye protection, gowns and gloves, and with hand hygiene.
Unintentional Injury from CPR to Persons Not in Cardiac Arrest
Last Full Review: ILCOR 2025
Last Update: 2020
CPR provided by laypersons and bystanders is critical to improving outcomes in out-of-hospital cardiac arrest (OHCA). Bystanders, however, may hesitate to start CPR for several reasons, including concern about transmission of infectious disease or concern that a person is not actually in cardiac arrest or that they may cause an injury with forceful chest compressions. In some cases, bystanders may be concerned about potential liability from their actions, particularly if they cause an injury. An updated systematic review by ILCOR looks at the incidence of unintentional injuries seen when CPR is provided to a person not in cardiac arrest.
Red Cross Guidelines
- Lay responders and healthcare professionals should begin cardiopulmonary resuscitation based on their assessment and without concern for causing unintentional physical injury to persons not in cardiac arrest.
Evidence Summary
A 2024 International Liaison Committee on Resuscitation (ILCOR) systematic review (Williamson et al. 2024, 100828) and Consensus on Science with Treatment Recommendations (CoSTR) (Williamson et al. 2024, 100828; Djärv et al. 2025, S250) sought evidence for clinical outcomes, including physical injury, in adults and children with out-of-hospital cardiac arrest (OHCA) following the provision of chest compressions by laypersons. This review was an update of a 2020 systematic review and CoSTR (Svavsrsdottir et al. 2021) but focused on layperson CPR. A single study (Ng et al. 2022, 266) was identified and added to the evidence from four studies included in 2020 (White et al. 2010, 91; Tanaka et al. 2014, 1751; Moriwaki et al. 2012, 3; Haley et al. 2011, 282). In total, the five studies with a total of 1,031 patients not in cardiac arrest who received CPR showed that seven (0.7 percent of the total) patients experienced unintentional physical injury. There were no deaths caused by CPR on patients not in cardiac arrest. Symptoms such as chest pain or discomfort from compressions were reported in 24 (2 percent) of patients.
The International Liaison Committee on Resuscitation made a strong recommendation that laypersons initiate CPR for presumed cardiac arrest without concerns of causing unintentional injury. A good practice statement recommends that other rescuers (e.g., trained bystanders, healthcare professionals, those with a duty to respond) initiate CPR for presumed cardiac arrest without concerns of causing unintentional injury to persons not in cardiac arrest (Williamson et al. 2024; Bray et al. 2025, S34).
Insights and Implications
The review noted a substantially lower incidence of chest wall bone fractures reported in the included studies than the incidence reported after CPR in patients who were in actual cardiac arrest. The authors surmised this may be due to a shorter duration of CPR (most often less than 5 minutes) provided by laypersons before being stopped by professional rescuers, although it could also reflect underreporting of injuries.
The risk of unintentional physical injury is quite low, and the potential survival benefit from providing CPR outweighs this risk. The Red Cross guidelines have been updated to include healthcare professionals in the recommendation to begin CPR based on assessment of cardiac arrest and without concern for causing unintentional physical injury.
Termination of Resuscitation Rules
Last Full Review: ILCOR 2020
Termination of resuscitation by prehospital professionals is often guided by a set of rules adopted by emergency medical service systems.
Red Cross Guidelines
- It is reasonable for prehospital systems to include termination of resuscitation rules in their medical protocols.
Evidence Summary
A systematic review by International Liaison Committee on Resuscitation (ILCOR) in 2020 evaluated the use of termination of resuscitation rules for their ability to reliably predict in-hospital outcomes of death and unfavorable neurologic outcome following out-of-hospital cardiac arrest (Greif et al. 2020, s222). Studies included were reported to describe the derivation and internal validation of individual termination of resuscitation rules, or the external validation of previously published termination of resuscitation rules. Only a single study addressed clinical validation of a termination of resuscitation rule. Based on the consensus of science from this review, ILCOR made a conditional recommendation for the use of termination of resuscitation rules to assist clinicians in deciding whether to discontinue resuscitation efforts out-of-hospital, or to transport to a hospital with ongoing cardiopulmonary resusitation (CPR) (Greif et al. 2020, s222).
Insights and Implications
Widespread implementation of termination of resuscitation rules following cardiac arrest has occurred in many emergency medical services (EMS) systems. These rules typically include criteria such as, an unwitnessed arrest by EMS of bystanders; no bystander CPR; no defibrillation delivered; and no return of spontaneous circulation. The ability to discontinue resuscitation has the potential to preserve the dignity of recently deceased, to reduce EMS transport rates and risks for EMS professionals, to reduce stress on healthcare resources, and to provide a significant savings in healthcare costs. The potential for misclassifying eventual survivors with termination of resuscitation rules is a legitimate concern for clinicians. A 2019 meta-analysis of nine different termination of resuscitation rules addressed this concern by evaluating the accuracy of several termination of resuscitation rules for out-of-hospital cardiac arrest (Ebell et al. 2019, 479). The Basic Life Support (BLS) and European Resuscitation Council termination of resuscitation rules were found in this meta-analysis to identify a large proportion of candidates for termination of resuscitation after out-of-hospital cardiac arrest (ERC, 95 percent; BLS, 97 percent) while having a very low rate of misclassifying eventual survivors (<0.1 percent), but it was felt that further prospective validation of the European Resuscitation Council termination of resuscitation was needed, along with comparative studies with the BLS termination of resuscitation rule (Ebell et al. 2019, 479).

