Early Access
Public Access Defibrillation Programs for Infants, Children and Adolescents
Last Full Review: ILCOR 2022; American Red Cross Scientific Advisory Council 2010 (Infant)
Last Update: 2023 (Infant)
Out-of-hospital cardiac arrest is rare in infants and children, and unlike adults, is less likely to be due to a primary cardiac event and more likely the result of a respiratory issue or trauma. Is there evidence to support the use of public access automated external defibrillators (AEDs) in pediatric out-of-hospital cardiac arrest?
Red Cross Guidelines
- Public access defibrillation may be used in infants, children and adolescents for out-of-hospital cardiac arrest. If available, pediatric-specific automated external defibrillator pads or electrical settings should be used for infants and children 8 years of age or younger or weighing 25 kilograms or less.
Evidence Summary
A 2022 systematic review (Atkins et al. 2022b, 100283) and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2022, e645, 1095; Atkins et al. 2022a) by the International Liaison Committee on Resuscitation (ILCOR) evaluated the evidence for the application of, or shock delivery from, an AED by lay rescuers to infants, children and adolescents with nontraumatic out-of-hospital cardiac arrest compared with standard care without AED application and use. Four observational studies were identified, including three from the Cardiac Arrest Registry to Enhance Survival (CARES) database (Naim et al. 2019, e012637; Naim et al. 2017, 133; Griffis et al. 2019, 126). Data from the CARES studies was used to calculate the relative risk of survival if an AED was applied and analyzed by age group for infants less than 1 year of age, children 1 to 12 years of age and adolescents from 13 to 18 years of age. The relative risk of survival to hospital discharge with a Cerebral Performance Category score of 1 to 2, and for survival to hospital discharge was found to be significantly improved with AED application in all age groups except for the under 1 year age group (Atkins et al. 2022a, 100283; Atkins et al. 2022b).
A weak recommendation was made by ILCOR suggesting the use of an AED by lay rescuers for all children over 1 year of age who have a nontraumatic out-of-hospital cardiac arrest (Wyckoff et al. 2022, e483; Atkins et al. 2022b). No recommendation was made for or against the use of an AED by lay rescuers for infants under 1 year of age with a nontraumatic out-of-hospital cardiac arrest. The authors noted the limited evidence available, including a small percentage of children (1.5 percent) from the CARES database who had an AED applied and a small percentage of children (3.7 percent) in the fourth observational study (Kiyohara et al. 2018, 890) who had a shock delivered. Only 12 patients in the under 1 year age group had an AED applied, with one survival. Because this may result in a false negative result, a recommendation was not made by ILCOR for this age group .
Insights and Implications
Cardiac arrest in children is commonly preceded by a respiratory event and hypoxemia. As would be expected, ventilations with compressions have been shown to be vitally important for successful resuscitation (Tobin et al. 2017, 39). The application of an AED may delay starting cardiopulmonary resuscitation (CPR) or increase pauses in CPR, which could be potentially detrimental. The review authors acknowledge this but note the relative risk was still significantly in favor of AED application (Wyckoff et al. 2022, e483; Atkins et al. 2022b). While out-of-hospital cardiac arrest is less common in infants and children than in adults, shockable rhythms do occur in this population.
Despite the lack of evidence in the ILCOR review to support the public use of AEDs for infants with out-of-hospital cardiac arrest, there is no evidence to suggest harm from their use. Although the application of an AED may cause a slight pause in CPR, that determinant is outweighed by the lifesaving benefit in infants and children with shockable rhythms.
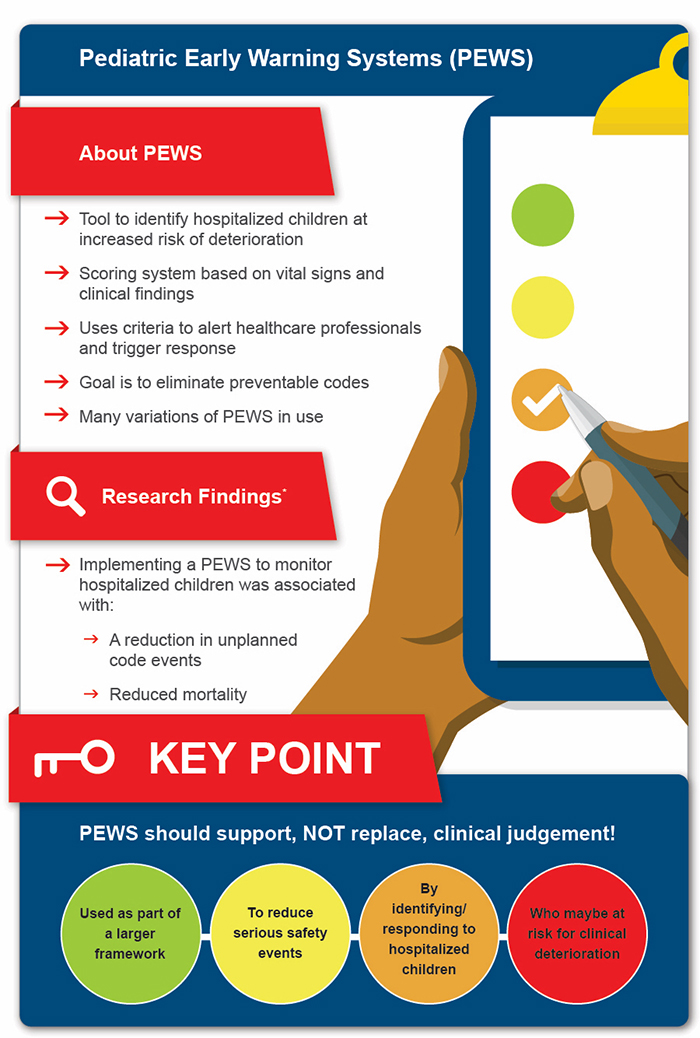
Pediatric Early Warning Systems
Last Full Review: ILCOR 2022
A significant percentage of in-hospital pediatric serious events and deaths have been shown to be associated with a failure to detect and respond to clinical deterioration (Burrus et al. 2021, e2020030346). This has led to the development of tools for use in the healthcare setting, including pediatric early warning systems (PEWS), to alert healthcare professionals to clinical deterioration through periodic observation of physiologic parameters, application of a scoring system and criteria for triggering communication and an appropriate response. Is there clinical evidence to support the use of PEWS?
Red Cross Guidelines
- Pediatric early warning systems may be used as part of a larger framework to reduce serious safety events by identifying and responding to hospitalized infants, children and adolescents who may either be at risk for deterioration or be deteriorating clinically.
Evidence Summary
A 2022 systematic review (Chong et al. 2022, 100262) and Consensus on Science with Treatment Recommendations (Wycoff et al. 2022, e483; Ong et al. 2022) by the International Liaison Committee on Resuscitation (ILCOR) evaluated the use of PEWS, with or without rapid response teams or medical emergency teams, in hospitalized infants, children and adolescents compared with standard care without a scoring system. The review included a single randomized controlled trial (Parshuram et al. 2018, 1002) and multiple cohort studies; the certainty of evidence was rated as very low across all outcomes due to very serious risk of bias and imprecision. No significant difference in mortality, cardiopulmonary arrest events or significant deterioration events was shown with the use of PEWS compared with no PEWS. However, there was a trend toward increased mortality in the pooled analysis for the no PEWS group and toward both increased cardiopulmonary arrests and increased significant clinical deterioration events with no PEWS. For the outcome of unplanned code events, a statistically significant increase in unplanned code events was demonstrated with no PEWS compared with the PEWS group (pooled IRR/RR, 1.73, 95% CI, 1.01–2.96). A weak recommendation by ILCOR suggests using PEWS to monitor hospitalized children with the aim of identifying those who may be deteriorating (Wycoff et al. 2022, e483; Ong et al. 2022).
Insights and Implications
Pediatric early warning systems are one component of an organization strategy used in many hospitals to help healthcare professionals recognize children who are either at risk for clinical deterioration or who are clinically deteriorating, using established criteria, and to accelerate an urgent response through a clear communication plan. Pediatric early warning systems should support, but not be a replacement for, clinical judgement. Many variations of PEWS exist, with a wide range of sensitivities and specificities for detecting clinical deterioration (Lambert at al. 2017, e014497) Other components of a rapid response system include having the necessary personnel and resources for response, such as a medical emergency team or rapid response team, that focuses on correcting the deteriorating child’s physiology, a process-monitoring and improvement plan, and an administrative structure to implement and support the system (Jagt 2013, 158; Troy et al. 2021, 399; Olasveengen et al. 2017, e424).
*Chong SL, Goh MSL, Ong GY, et al. Do paediatric early warning systems reduce mortality and critical deterioration events among children? A systematic review and meta-analysis. Resusc Plus. Sep 2022;11:100262. doi:10.1016/j.resplu. 2022.100262

