Neuroprognostication After Cardiac Arrest and ROSC: Prediction of Good Neurological Outcome
Glasgow Coma Scale Motor Score
Last Full Review: ILCOR 2023
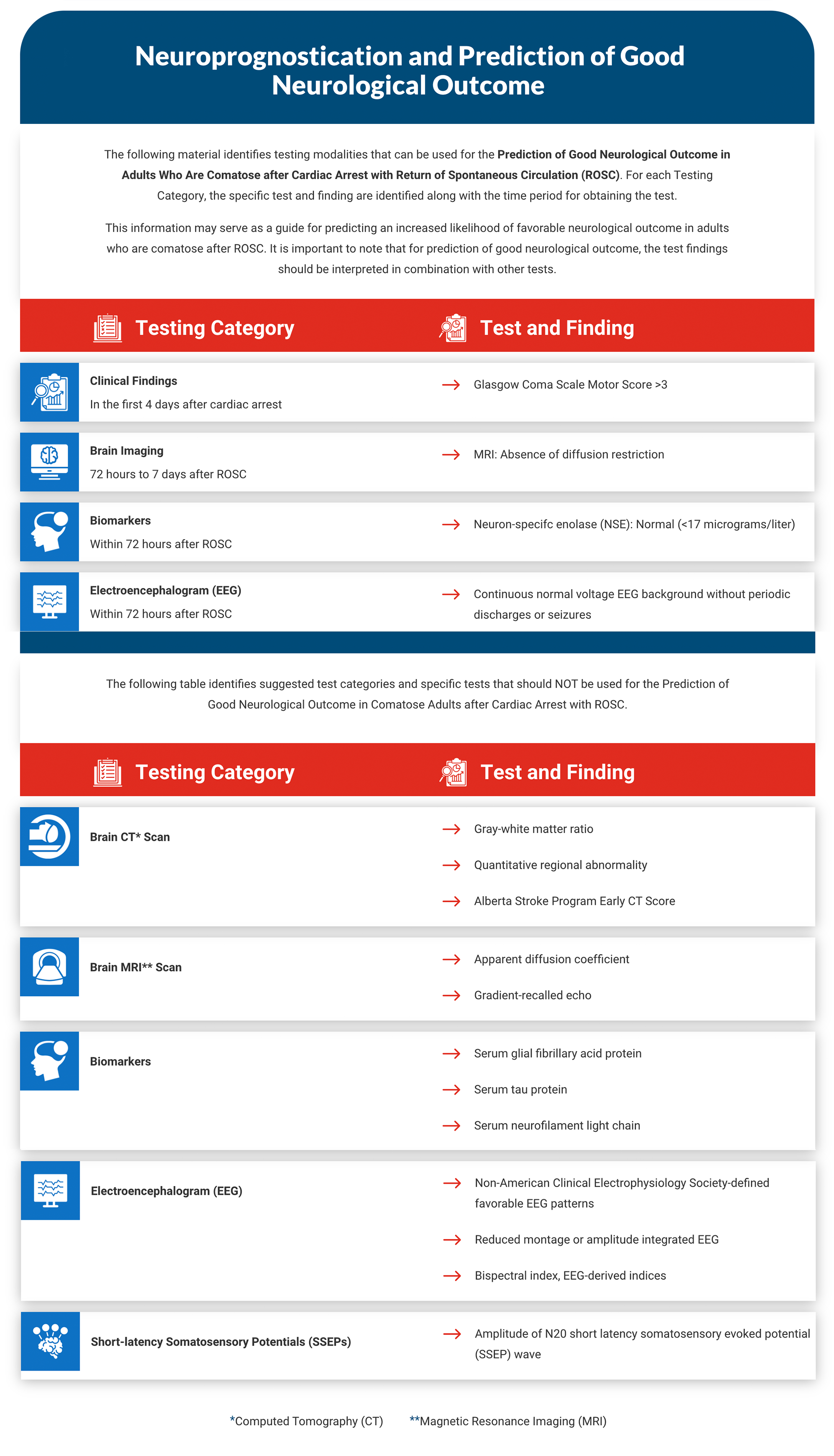
The brain is prone to hypoxic injury during cardiac arrest and following the return of spontaneous circulation (ROSC). Therefore, some patients will develop global cerebral edema followed by herniation and brain death within 24 hours, while others will remain comatose and are at risk for severe neurological injury. Prognostication has been used to help families and physicians make decisions to limit or withdraw life support when unfavorable neurological outcomes are expected. In 2020, a systematic review (Sandroni et al. 2020, 1803) assessed the ability to predict poor neurological outcome in comatose adult survivors from cardiac arrest using multiple modalities—including clinical examination, blood biomarkers, electrophysiology and neuroimaging. The studies identified in the review were considered by the International Liaison Committee on Resuscitation (ILCOR) with four separate Consensus on Science with Treatment Recommendations (CoSTR) statements published on neuroprognostication using clinical examination, neurophysiological tests, blood biomarkers and neuroimaging (Berg et al. 2020, S92). A second part of this review looks at modalities that can be used to predict favorable neurological outcome in comatose adults following ROSC.
This portion of the review summarizes the evidence for use of the Glasgow Coma Scale motor score for prognostication of favorable neurological outcome. The existing Red Cross guidelines for prediction of poor neurological outcome are not impacted by the current review and new guidelines below.
Red Cross Guidelines
- For adults who are comatose after cardiac arrest, assessment of the Glasgow Coma Scale motor score in the first 4 days after cardiac arrest may be considered to identify patients with a score higher than 3, which may indicate an increased likelihood of favorable outcome.
Evidence Summary
A systematic review from 2022 by Sandroni et al. (Sandroni et al. 2022, 389) considered evidence for the prediction of good neurological outcome in adults (16 years of age and older) who are comatose after resuscitation from in-hospital or out-of-hospital cardiac arrest, regardless of target temperature. This systematic review was used by ILCOR in an adolopment (Schünemann et al. 2017, 101) process with a literature search updated through May 20, 2022. Outcomes included prediction of good neurological outcome defined as a Cerebral Performance Category score of 1 or 2, or modified Rankin score of 1 to 3 at hospital discharge or 1 month later. Evidence that was identified was separated by testing modalities into Glasgow Coma Scale motor score, imaging, biomarkers and the use of electroencephalography and somatosensory evoked potential tests (testing of brain and spinal cord responses elicited by sensory stimuli). Evidence from each modality is reported by sensitivity and specificity for predicting favorable neurological outcome, with sensitivity reflecting the percentage of patients with a favorable outcome who will have a favorable (positive) test, while specificity reflects the percentage of patients with an unfavorable outcome who will have an unfavorable (negative) test.
A CoSTR (Skrifvars et al. 2023; Berg et al. 2023) by ILCOR summarized evidence identified in the systematic review for the use of the Glasgow Coma Scale motor score evaluated within 4 days in adults who are comatose after resuscitation from cardiac arrest, and regardless of target temperature. The systematic review (Sandroni et al. 2022, 389) identified two observational studies, and no additional studies were identified in the updated literature search.
The first study (Moseby-Knappe et al. 2020, 1852), with 342 out-of-hospital cardiac arrest patients, reported that a Glasgow Coma Scale motor score greater than 3 on day 4 after cardiac arrest predicted favorable outcome at 6 months (specificity, 84%; 95% CI, 79%–88%; sensitivity, 77%; 95% CI, 67%–85%). A Glasgow Coma Scale motor score of 3 to 5 on day 4 predicted favorable outcome—with a specificity of 72% (95% CI, 66%–77%) and sensitivity of 96% (95% CI, 93%–97%).
A second study, (Hifumi et al. 2015, 2201) with 302 out-of-hospital cardiac arrest patients, reported that a Glasgow Coma Scale motor score of 4 to 5 on intensive care unit admission predicted a favorable outcome at 3 months (specificity, 98%; 95% CI, 93%–99%; sensitivity, 12%; 95% CI, 7%–17%). Very low-certainty evidence from these two studies supports a weak treatment recommendation by ILCOR to assess the Glasgow Coma Scale motor score in the first 4 days after cardiac arrest to identify patients with a score higher than 3, which may indicate an increased likelihood of favorable outcome (Skrifvars et al. 2023; Berg et al. 2023).
Insights and Implications
The Red Cross guidelines for predicting good neurological outcome are informed by the ILCOR systematic review and treatment recommendations. While assessment of the Glasgow Coma Scale motor score may be useful for recognizing comatose patients who should undergo functional and structural testing for prognostication, it is important to consider that the use of sedatives, such as midazolam and analgesics, may confound the assessment. Other confounders may include electrolyte abnormalities, encephalopathy, severe metabolic acidosis, multiorgan failure, unrecognized seizures and traumatic brain injury.
Prognostication requires both functional (i.e., neurological examination) and structural test information considered over time and with consideration of confounders.
.
Brain Imaging
Last Full Review: ILCOR 2023
The brain is prone to hypoxic injury during cardiac arrest and following the return of spontaneous circulation (ROSC). Therefore, some patients will develop global cerebral edema followed by herniation and brain death within 24 hours, while others will remain comatose and are at risk for severe neurologic injury. Prognostication has been used to help families and physicians make decisions to limit or withdraw life support when unfavorable neurological outcomes are expected. In 2020, a systematic review (Sandroni et al. 2020, 1803) assessed the ability to predict poor neurological outcome in comatose adult survivors from cardiac arrest using multiple modalities including clinical examination, blood biomarkers, electrophysiology and neuroimaging. The studies identified in the review were considered by the International Liaison Committee on Resuscitation (ILCOR) with four separate Consensus on Science with Treatment Recommendations (CoSTR) statements published on neuroprognostication using clinical examination, neurophysiological tests, blood biomarkers and neuroimaging (Berg et al. 2020, S92). A second part of this review looks at modalities that can be used to predict favorable neurological outcome in comatose adults following ROSC.
This portion of the review summarizes the evidence for use of brain imaging for prognostication of favorable neurological outcome. The existing Red Cross guidelines for prediction of poor neurological outcome are not impacted by the current review and new guidelines below.
Red Cross Guidelines
- For adults who are comatose after cardiac arrest, it is suggested to not use gray-white matter ratio, quantitative regional abnormality and the Alberta Stroke Program Early Computed Tomography Score on brain computed tomography to predict good neurological outcome.
- For adults who are comatose after cardiac arrest, it is reasonable to consider using the absence of diffusion restriction on magnetic resonance imaging between 72 hours and 7 days after return of spontaneous circulation in combination with other tests for prediction of good neurological outcome.
- For adults who are comatose after cardiac arrest, it is suggested to not use either apparent diffusion coefficient or absence of gradient-recalled echo changes on brain magnetic resonance imaging for prediction of good neurological outcome.
Evidence Summary
A systematic review from 2022 by Sandroni et al. (Sandroni et al. 2022, 389) considered evidence for prediction of good neurological outcome in adults (16 years of age and older) who are comatose after resuscitation from in-hospital or out-of-hospital cardiac arrest, regardless of target temperature. This review was used by ILCOR in an adolopment process (Schünemann et al. 2017, 101), with a literature search updated through May 20, 2022. Outcomes included prediction of good neurological outcome defined as a Cerebral Performance Category score of 1 or 2, or modified Rankin score of 1 to 3 at hospital discharge or 1 month later. Evidence identified was separated by testing modalities into Glasgow Coma Scale motor score, imaging, biomarkers and use of electroencephalography and somatosensory evoked potential tests (testing of brain and spinal cord responses elicited by sensory stimuli). Evidence from each modality is reported by sensitivity and specificity for predicting favorable neurological outcome, with sensitivity reflecting the percentage of patients with a favorable outcome who will have a favorable (positive) test, while specificity reflects the percentage of patients with an unfavorable outcome who will have an unfavorable (negative) test.
Six studies were included in the evidence evaluation for the ILCOR CoSTR (Sandroni et al. 2023; Berg et al. 2023). Meta-analysis was not possible due to heterogeneity between studies. A single study (Lee et al. 2017, 1628) assessed the use of brain computed tomography (CT) for prognostication of favorable neurological outcomes in 67 patients using a gray matter to white matter ratio greater than 1.25, a quantitative regional abnormality score of 5 or less and an Alberta Stroke Program Early Computed Tomography-b Score (ASPECTS-b) of 15 or greater. The highest sensitivity (75%; 95% CI, 50.9%–91.3%) and specificity (89%; 95% CI, 76.9%–96.0%) of these measures was observed with an ASPECTS-b of 15 or higher at 124.5 minutes (+/- 59.9 minutes) after ROSC for prediction of good neurological outcome at 1 month.
The use of diffusion-weight imaging on brain magnetic resonance imaging (MRI) for prognostication was evaluated in five observational studies, with imaging between 3.1 hours post-ROSC to 8 days. In one study, (Oh et al. 2019, 224) absence of restricted diffusion in the cortex or deep grey matter on diffusion-weight imaging immediately after rewarming predicted good neurological outcome at 6 months with high specificity (94.9%; 95% CI, 88.5%–98.3%) and sensitivity (72%, 95% CI, 54.8%–85.8%).
In another study (Jang et al. 2019, 142), the absence of restricted diffusion on MRI at 77.6 hours after ROSC had a reported sensitivity of 91.7% (95% CI, 61.5%–99.8%) and specificity of 92.6% (95% CI, 75.7%–99.1%) for prediction of good outcome at 6 months.
One small study (Park et al. 2020, 39) reported the absence of cortical necrosis on MRI at 3.1 hours post-ROSC had a 60% specificity (95% CI, 32.3%–83.7%) and 100% sensitivity (95% CI, 86.7%–100%) for predicting good outcome at 6 months. In the same study, the absence of cortical necrosis on MRI at 77.6 hours after ROSC reported a specificity of 93.3% (95% CI, 68.1%–99.8%) and 100% sensitivity (95% CI, 86.7%–100%) for predicting a good outcome at 6 months. Other MRI measures evaluated in the systematic review, such as fluid-attenuated inversion recovery lesions in the cortex, gray nuclei, cerebellum and pons—measured at 8 or less days—had variable sensitivities and specificities. Very low-certainty evidence was identified for use of T2-weighted gradient-recalled echo and for use of apparent diffusion coefficient on MRI, with each modality limited to a single, small study.
The ILCOR treatment recommendations (Sandroni et al. 2023; Berg et al. 2023) suggest using the absence of diffusion restriction on MRI between 72 hours and 7 days after ROSC in combination with other tests for prediction of good neurological outcome of adults who are comatose after cardiac arrest.
Additionally, ILCOR provides a weak recommendation suggesting against the use of gray-white matter ratio, quantitative regional abnormality and the Alberta Stroke Program Early CT Score on brain CT to predict good neurological outcome in patients who are comatose after cardiac arrest.
Weak recommendations suggest against using apparent diffusion coefficient and gradient- recalled echo on brain MRI to predict good neurological outcome in patients who are comatose after cardiac arrest (Sandroni et al. 2023; Berg et al. 2023).
Insights and Implications
The Red Cross guidelines for predicting good neurological outcome are informed by the ILCOR systematic review and treatment recommendations. Cytotoxic edema of the brain due to anoxia affects the gray matter preferentially and reduces the gray/white ratio toward a value of 1 on CT scan. This has been used for prediction of poor neurological outcome, but in the current review, only a single study provided evidence showing that a high gray/white ratio, low quantitative regional attenuation score or a high Alberta Stroke Program Early CT score predicted good neurological outcome. The most consistent findings from the studies included in the systematic review suggest that absence of cortical diffusion weighted imaging changes in the cortex or deep gray matter on MRI (i.e., absence of visible cytotoxic edema) predicts good neurological outcome at 72 hours post-arrest with high (greater than 80 percent) specificity.
Biomarkers
Last Full Review: ILCOR 2023
The brain is prone to hypoxic injury during cardiac arrest and following the return of spontaneous circulation (ROSC). Therefore, some patients will develop global cerebral edema followed by herniation and brain death within 24 hours, while others will remain comatose and are at risk for severe neurological injury. Prognostication has been used to help families and physicians make decisions to limit or withdraw life support when unfavorable neurological outcomes are expected.
In 2020, a systematic review (Sandroni et al. 2020, 1803) assessed the ability to predict poor neurological outcome in comatose adult survivors from cardiac arrest using multiple modalities including clinical examination, blood biomarkers, electrophysiology and neuroimaging. The studies identified in the review were considered by the International Liaison Committee on Resuscitation (ILCOR) with four separate Consensus on Science with Treatment Recommendations (CoSTR) statements published on neuroprognostication using clinical examination, neurophysiological tests, blood biomarkers and neuroimaging (Berg et al. 2020, S92). A second part of this review looks at modalities that can be used to predict favorable neurological outcome in comatose adults following ROSC.
This portion of the review summarizes the evidence for use of brain injury biomarkers for prognostication of favorable neurological outcome. The existing Red Cross guidelines for prediction of poor neurological outcome are not impacted by the current review and new guidelines below.
Red Cross Guidelines
- Use of a normal neuron-specific enolase biomarker level (less than 17 micrograms per liter) within 72 hours after return of spontaneous circulation may be considered in adults who are comatose after cardiac arrest, in combination with other tests, for predicting favorable neurological outcome.
- For adults who are comatose after cardiac arrest, it is suggested to not use serum levels of glial fibrillary acid protein, serum tau protein or serum neurofilament light chain for predicting favorable neurological outcome.
Evidence Summary
A systematic review from 2022 by Sandroni et al. (Sandroni et al. 2022, 389) looked at prognostication of good neurological outcome in adults (16 years of age and older) who are comatose after resuscitation from in-hospital or out-of-hospital cardiac arrest, regardless of target temperature. This review was used by ILCOR in an adolopment process, (Schünemann et al. 2017, 101) with a literature search updated through May 20, 2022. Outcomes included prediction of good neurological outcome defined as a Cerebral Performance Category score of 1 or 2, or modified Rankin score of 1 to 3 at hospital discharge or 1 month later. Evidence identified was separated by testing modalities into Glasgow Coma Scale motor score, imaging, biomarkers, use of electroencephalography and somatosensory evoked potential tests (testing of brain and spinal cord responses elicited by sensory stimuli). Evidence from each modality is reported by sensitivity and specificity for predicting favorable neurological outcome, with sensitivity reflecting the percentage of patients with a favorable outcome who will have a favorable (positive) test, while specificity reflects the percentage of patients with an unfavorable outcome who will have an unfavorable (negative) test.
Various brain injury biomarkers have been studied to determine if a normal or low level of the biomarker is predictive of good outcome after cardiac arrest. Six observational studies from the original systematic review and updated literature search were included in an ILCOR CoSTR (Berg et al. 2023). Heterogeneity between studies prevented meta-analyses. Of the various brain injury biomarkers, neuron-specific enolase (NSE) was investigated in the most studies (four) and with a total of 2141 patients. Samples were taken between 24 hours and 72 hours. Blood NSE values within the upper limit of the normal range at 24 hours were reported in two studies (Moseby-Knappe et al. 2020, 1852; Zellner et al. 2013, 1382) to predict favorable neurological outcome at 6 months. Specificities were 85 percent and 89 percent respectively, and sensitivities 46 percent and 26 percent. Specificities were similar at 48 hours, while sensitivities were somewhat higher than those at 24 hours. At 72 hours, one study (Moseby-Knappe et al. 2020, 1852) reported that a normal NSE level predicted good neurological outcome at 6 months with a specificity of 80 percent and sensitivity of 75 percent.
Others novel biomarkers evaluated in the systematic review included S100 calcium-binding protein B, glial fibrillary acid protein, serum tau protein, serum neurofilament light chain (NfL) and ubiquitin carboxy-germinal hydrolaste-1. However, these biomarkers require measurement in specialized laboratories and have variable threshold levels for predicting a good functional outcome.
The International Liaison Committee on Resuscitation provides a weak treatment recommendation to use normal NSE (less than 17 micrograms per liter) within 72 hours after ROSC, in combination with other tests, for predicting favorable neurological outcome in adults who are comatose after cardiac arrest. In addition, ILCOR suggests against using serum levels of glial fibrillary acid protein, serum tau protein or NfL in clinical practice for predicting favorable neurological outcome in adults who are comatose after cardiac arrest (Berg et al. 2023).
Insights and Implications
The Red Cross guidelines for predicting good neurological outcome are informed by the ILCOR systematic review and CoSTR. Neuron-specific enolase is an enzyme found in the cytoplasm of neurons and neuroendocrine cells and is released with brain injury or hemolysis. The best evidence in the ILCOR systematic review of brain injury biomarkers for prediction of favorable outcome after cardiac arrest was for the use of NSE, based on the number of studies and patients included, and consistency between study threshold values. A normal blood value of NSE at 24 hours to 72 hours after ROSC was shown in most studies to predict good neurological outcome—with greater than 80 percent specificity and greater than 40 percent sensitivity. However, NSE testing may not be available at many hospitals. Turnaround time may be long, and there are no calibration standards between laboratories. False-positive elevations of NSE values may be seen with hemolysis. While the specificity of predicting a good outcome is high with a normal NSE, the systematic review author points out that post-cardiac arrest patients may die, despite a normal NSE value, due to a secondary deterioration after regaining consciousness (Sandroni et al. 2022, 389).
Electroencephalogram
Last Full Review: ILCOR 2023
The brain is prone to hypoxic injury during cardiac arrest and following the return of spontaneous circulation (ROSC). Therefore, some patients will develop global cerebral edema followed by herniation and brain death within 24 hours, while others will remain comatose and are at risk for severe neurological injury. Prognostication has been used to help families and physicians make decisions to limit or withdraw life support when unfavorable neurological outcomes are expected. In 2020, a systematic review (Sandroni et al. 2020, 1803) assessed the ability to predict poor neurological outcome in comatose adult survivors from cardiac arrest using multiple modalities including clinical examination, blood biomarkers, electrophysiology and neuroimaging. The studies identified in the review were considered by the International Liaison Committee on Resuscitation (ILCOR) with four separate Consensuses on Science with Treatment Recommendations (CoSTR) statements published on neuroprognostication using clinical examination, neurophysiological tests, blood biomarkers and neuroimaging (Berg et al. 2020, S92). A second part of this review looks at modalities that can be used to predict favorable neurological outcome in comatose adults following ROSC.
This portion of the review summarizes the evidence for the use of an electroencephalogram (EEG), reduced montage and/or amplitude-integrated EEG and EEG-derived indices, such as bispectral index, for prognostication of favorable neurological outcome. The existing Red Cross guidelines for prediction of poor neurological outcome are not impacted by the current review and new guidelines below.
Red Cross Guidelines
- The use of a continuous or nearly continuous normal voltage electroencephalogram (EEG) background without periodic discharges or seizures within 72 hours from return of spontaneous circulation, in combination with other indices, may be considered for predicting good outcome in patients who are comatose after cardiac arrest.
- For adults who are comatose after cardiac arrest, it is suggested to not use heterogeneous, non-American Clinical Electrophysiology Society-defined favorable EEG patterns, or other EEG metrics—including reduced montage or amplitude integrated EEG, and bispectral index or EEG-derived indices—to predict good neurological outcome.
Evidence Summary
A systematic review from 2022 by Sandroni et al (Sandroni et al. 2022, 389) evaluated evidence for prognostication of good neurological outcome in adults (16 years of age and older) who are comatose after resuscitation from in-hospital or out-of-hospital cardiac arrest, regardless of target temperature. This review was used by ILCOR in an adolopment process (Schünemann et al. 2017, 101), with a literature search updated through May 20, 2022. Outcomes included prediction of good neurological outcome defined as a Cerebral Performance Category score of 1 or 2, or modified Rankin score of 1 to 3 at hospital discharge or 1 month later. Evidence identified was separated by testing modalities into Glasgow Coma Scale motor score, imaging, biomarkers, use of EEG and somatosensory evoked potential tests (testing of brain and spinal cord responses elicited by sensory stimuli). Evidence from each modality is reported by sensitivity and specificity for predicting favorable neurological outcome, with sensitivity reflecting the percentage of patients with a favorable outcome who will have a favorable (positive) test, while specificity reflects the percentage of patients with an unfavorable outcome who will have an unfavorable (negative) test.
A total of 24 studies from the systematic review (Sandroni et al. 2022, 389) were included in an ILCOR CoSTR (Hirsch et al. 2022; Berg et al. 2023) that summarized evidence for use of an EEG, reduced montage and/or amplitude-integrated EEG and EEG-derived indices, such as bispectral index. A favorable EEG pattern in the first 5 days after ROSC to predict good neurological outcome was the focus of 12 studies in the review. A favorable pattern was defined as a continuous or nearly continuous background without superimposed abundant (greater than 50 percent periodic discharges or abundant spike-wave) or generalized periodic discharged or seizures. Criteria for the superimposed discharges and the background varied slightly across the studies and can be found in the online CoSTR (Hirsch et al. 2022).
Because of variations in definitions, studies were grouped and summarized based on the definitions. A summary of the sensitivities and specificities based on the EEG criteria, timing of testing and numbers of enrollees is available in the online CoSTR (Hirsch et al. 2022). Most of the 12 studies reviewed reported a specificity of greater than 80 percent and greater than 50 percent sensitivity, have consistency of the background definition and use terminology from or compatible with the American Clinical Electrophysiology Society. An additional six studies confirmed the ability of a continuous, nearly continuous, discontinuous, normal and low-voltage EEG background without seizures or discharges to predict neurological outcomes, but evidence supporting these patterns was judged by ILCOR as insufficient for recommending their use. A few additional studies in the systematic review evaluated use of amplitude-integrated EEG or EEG-derived indices, such as bispectral index or cerebral recovery index. The limited evidence for these indices and concern that these techniques do not allow or allow only a limited morphologic assessment of the original EEG signal led to a recommendation against their use.
The Treatment Recommendations stemming from this CoSTR include (Hirsch et al. 2022; Berg et al. 2023):
- A weak recommendation that suggests using a continuous or nearly continuous normal voltage EEG background without periodic discharges or seizures within 72 hours from ROSC, in combination with other indices, to predict good outcome in patients who are comatose after cardiac arrest.
- A weak recommendation that suggests against using heterogeneous, non-American Clinical Electrophysiology Society-defined favorable EEG patterns to predict good neurological outcome after cardiac arrest.
- A weak recommendation that suggests against the use of other EEG metrics—including reduced montage or amplitude integrated EEG, and bispectral index or EEG-derived indices—to predict good outcome in patients who are comatose after cardiac arrest.
There is insufficient evidence to recommend for or against using a low voltage or a discontinuous EEG background on days 0 to 5 from ROSC to predict good neurological outcome after cardiac arrest.
Insights and Implications
The Red Cross guidelines for predicting good neurological outcome are informed by the ILCOR CoSTR. A continuous or nearly continuous normal voltage EEG background without seizures or abundant or generalized periodic discharges was consistent across 12 studies, with greater than 80 percent specificity and greater than 50 percent sensitivity for most studies. The use of sedatives is a potential confounder when using an EEG for prognostication since the amplitude may be suppressed and continuity of the EEG decreased. The systematic review (Sandroni et al. 2022) did not assess the time-to-recovery of a favorable EEG background. After ROSC, EEG background is suppressed, with the patterns evolving over time from more malignant appearance to more benign. The sooner a favorable EEG pattern develops appears to be associated with a favorable prognosis (Oh et al. 2015, 1094; Westhall et al. 2018, 1660).
Short-latency Somatosensory Evoked Potential
Last Full Review: ILCOR 2023
The brain is prone to hypoxic injury during cardiac arrest and following the return of spontaneous circulation (ROSC). Therefore, some patients will develop global cerebral edema followed by herniation and brain death within 24 hours, while others will remain comatose and are at risk for severe neurologic injury. Prognostication has been used to help families and physicians make decisions to limit or withdraw life support when unfavorable neurological outcomes are expected. In 2020, a systematic review (Sandroni et al. 2020, 1803) assessed the ability to predict poor neurological outcome in comatose adult survivors from cardiac arrest using multiple modalities including clinical examination, blood biomarkers, electrophysiology and neuroimaging. The studies identified in the review were considered by the International Liaison Committee on Resuscitation (ILCOR) with four separate Consensuses on Science with Treatment Recommendations (CoSTR) statements published on neuroprognostication using clinical examination, neurophysiological tests, blood biomarkers and neuroimaging (Berg et al. 2020, S92). A second part of this review looks at modalities that can be used to predict favorable neurological outcome in comatose adults following ROSC.
This portion of the review summarizes the evidence for use of short-latency somatosensory evoked potential tests for prognostication of favorable neurological outcome. The existing Red Cross guidelines for prediction of poor neurological outcome are not impacted by the current review and new guidelines below.
Red Cross Guidelines
- For adults who are comatose after cardiac arrest, it is suggested to not use the amplitude of the negative peak at 20 milliseconds short latency somatosensory evoked potential (SSEP N20) wave to predict good neurological outcome.
Evidence Summary
A systematic review from 2022 by Sandroni et al. (Sandroni et al. 2022, 389) looked at prediction of good neurological outcome in adults (16 years of age and older) who are comatose after resuscitation from in-hospital or out-of-hospital cardiac arrest, regardless of target temperature. This review was used by ILCOR in an adolopment process (Schünemann et al. 2017, 101), with a literature search updated through May 20, 2022. Outcomes included prediction of good neurological outcome defined as a Cerebral Performance Category score of 1 or 2, or modified Rankin score of 1 to 3 at hospital discharge or 1 month later. Evidence identified was separated by testing modalities into Glasgow Coma Scale motor score, imaging, biomarkers, use of encephalography and somatosensory evoked potentials (SSEPs [testing of brain and spinal cord responses elicited by sensory stimuli]). Evidence from each modality is reported by sensitivity and specificity for predicting favorable neurological outcome, with sensitivity reflecting the percentage of patients with a favorable outcome who will have a favorable (positive) test, while specificity reflects the percentage of patients with an unfavorable outcome who will have an unfavorable (negative) test.
This section of the systematic review (Sandroni et al. 2022, 389) considered the assessment of SSEP negative peak at 20 milliseconds (N20) wave amplitude within 1 week of ROSC for the prediction of good neurological outcome defined by Cerebral Performance Category score of 1 or 2, or a modified Rankin score of 0 to 3 at hospital discharge or 1 month later. Four studies investigating SSEPs were evaluated in the original systematic review, and one additional identified with the updated literature search was included in the ILCOR CoSTR (International Liaison Committee on Resuscitation 2023; Berg et al. 2023b). Meta-analyses were not performed due to inconsistency in N20 amplitude thresholds and timing of assessment.
The amplitude reported in studies was calculated in microvolts as the difference between the voltage of the N20 negative wave and the voltage of the following positive deflection 25 milliseconds after stimulation (P25) wave (N20-P25), although the baseline N20 amplitude was occasionally used if it was larger than the N20-P25 difference. The N20 amplitude threshold used for predicting good neurological outcome at 6 months after cardiac arrest varied widely across studies, from 2.31 microvolts to as high as 10 microvolts. Sensitivities and specificities likewise varied considerably. Overall, an N20 amplitude above 4.0 microvolts threshold had a reported specificity of greater than 90 percent for prediction of good neurological outcome.
A weak recommendation by ILCOR suggests against using the amplitude of the N20 SSEP wave to predict good neurological outcome of adults who are comatose after cardiac arrest (International Liaison Committee on Resuscitation 2023; Berg et al. 2023b).
Insights and Implications
The Red Cross guidelines for predicting good neurological outcome are informed by the ILCOR systematic review and CoSTR. The CoSTR authors note that observational studies have shown that sedative agents, such as midazolam, decrease the N20 amplitude. In addition, methods to calculate the N20 amplitude were inconsistent across studies, and the optimal timing for predicting good outcome using SSEP amplitude has yet to be determined (International Liaison Committee on Resuscitation 2023; Berg et al. 2023b).
A somatosensory evoked potential test is performed by stimulating the hand with electricity and tracing the nerve impulse to the sensory cortex of the brain. If the impulse does not reach the cortex, this indicates cortical damage, with an absent N20 wave. However, in patients with a cervical spinal cord injury, the signals from the SSEP may not reach the cortex and the test cannot be used.
