Training and Education
CPR Coaching During Adult and Pediatric Cardiac Arrest
Last Full Review: ILCOR 2025
The use of a cardiopulmonary resuscitation (CPR) coach as a member of adult and pediatric resuscitation teams has been proposed to improve adherence to CPR guidelines, to enhance CPR quality metrics and to provide cognitive offloading for team leaders (Lin et al. 2023, 100400; Buyck et al. 2021, 100058; Cheng et al. 2018, 33). Responsibilities may include providing real-time feedback on chest compression and ventilation quality, coordinating provider switches and assisting in minimizing interruptions during resuscitation. This topic was first review systematically by the International Liaison Committee on Resuscitation (ILCOR) in 2025.
Red Cross Guidelines
- The inclusion of a cardiopulmonary resuscitation coach on a resuscitation team may be considered in settings where there are adequate resources and implementation planning to include role definition, training and team integration.
Evidence Summary
A 2025 systematic review (Lauridsen et al. 2025, 100868) and Consensus on Science with Treatment Recommendations (CoSTR) (Lauridsen et al. 2024; Greif et al. 2025, S205) sought to evaluate the effect of having a CPR coach as part of a resuscitation team managing adult or pediatric cardiac arrest on outcomes of CPR performance, guideline adherence, teamwork, provider workload and patient survival.
Of the studies included in the review, one study (Infinger et al. 2014, 1752) focused on CPR coaches in a clinical setting while the remainder were simulation studies (Cheng et al. 2018, 33; Jones et al. 2021, e10707; Tofil et al. 2020, e274; Kessler et al. 2021, 345; Buyck et al. 2021, 100058; Badke et al. 2020, 100035). The one clinical study (Infinger et al. 2014, 1752) found that implementation of a CPR coach improved the fraction of compressions delivered and adequate depth from 69.8 percent to 80.4 percent, increased compression depth (43.6 millimeters [mm] to 47.2 mm) and reduced the time to defibrillation from 13.2 seconds to 7.2 seconds (Lauridsen et al. 2024; Greif et al. 2025, S205). The evidence for all outcomes in this study was very low certainty, and no P values or confidence intervals were reported for comparisons. Outcomes of adherence to guidelines in a clinical setting and patient survival were not reported.
All simulation studies suggested improved CPR quality and guideline adherence with the use of a CPR coach. One simulation study (Tofil et al. 2020, e274) reported that chest compressors had lower mental demand in a coached team but higher physical demand.
A weak recommendation from ILCOR (Lauridsen et al. 2024; Greif et al. 2025, S205), based on very low-certainty evidence, recommends considering the inclusion of a CPR coach as a member of the resuscitation team during cardiac arrest resuscitation in settings with adequate staffing.
Insights and Implications
The evidence supporting the ILCOR recommendation included only one clinical study that failed to report statistical significance for outcomes described, and one randomized simulation-based trial with five other simulation studies that were based on the same randomized controlled trial. Several clinical outcomes were not reported in the clinical study. Direct evidence linking CPR coaches to improved survival or neurological outcomes in real patients is still limited.
The review does not consider the additional resources needed and training required for effectiveness of a CPR coach, including knowledge of CPR metrics, communication and feedback delivery. There is the potential to degrade performance with untrained CPR coaches (Badke et al. 2020, 100035). The presence of an additional person can create space and logistical obstacles in small spaces, and a CPR coach may provide overlapping instructions or conflicting commands if a team leader is already providing feedback. In some settings or low-staffed environments, assigning a dedicated CPR coach may not be feasible. The Red Cross guidelines reflect the limited evidence to support a recommendation for use of a CPR coach.
First Aid Education in Primary and Secondary Schools
Last Full Review: American Red Cross Scientific Advisory Council Position 2020
First aid education is considered mandatory in primary and secondary schools in many countries. An evidence-based position statement supporting first aid education in primary and secondary schools was completed by the American Red Cross Scientific Advisory Council in 2020 (American Red Cross Scientific Advisory Council 2020c).
Red Cross Guidelines
- First aid and cardiopulmonary resuscitation education should be provided in primary and secondary schools.
Evidence Summary
Multiple studies have shown that young children can successfully acquire and retain first aid skills (Bollig, Myklebust, and Østringen 2011, 13; Banfai et al. 2017, 526; Bollig, Wahl, and Svendsen 2009, 689; Uray et al. 2003, 211). Children as young as 4 years old can assess a victim’s consciousness and breathing, call the correct emergency telephone number and give the pertinent information, and place the person in a recovery position (Bollig, Wahl, and Svendsen 2009, 689; Uray et al. 2003, 211; Ammirati et al. 2014, e005848). Instruction has been provided in short sessions (less than 1 hour) or as single multi-hour sessions taught by classroom teachers or first aid instructors. There is evidence that children can learn first aid knowledge and skills from web-based platforms, with no reported adverse consequences of first aid education in younger age groups.
Insights and Implications
Increasing exposure to first aid education by providing it in schools will help to integrate essential skills into daily life for much of the population and may increase bystander willingness to help in those crucial first moments. Additionally, providing first aid within a public-school setting makes it accessible to a large portion of the population and may help decrease health disparities in underserved communities.
Opioid Overdose First Aid Education
Last Full Review: ILCOR 2021
A 2020 position statement by the Red Cross (American Red Cross Scientific Advisory Council: Education 2020a) recognizes the declaration by the United States Department of Health and Human Services of the opioid epidemic as a public health emergency. The Red Cross supports the availability of community opioid education and naloxone distribution programs to reduce mortality from opioid overdose and to reduce the burden on society.
Red Cross Guidelines
- Overdose education programs and naloxone distribution programs should be widely available to the community.
- Overdose education programs should include training on naloxone administration, the potential complications of naloxone administration and the management of these complications.
Evidence Summary
A 2021 scoping review by the International Liaison Committee on Resuscitation (Pellegrino, Krob, and Orkin 2021, e12454) sought literature related to education of first aid providers on the response and care of an individual with an opioid overdose emergency, as compared with nonspecialized first aid education. Outcomes that were sought included any clinical or educational outcomes. From the initial 2,089 records identified, 59 studies were included in an observational synthesis and eight studies were included in meta-analysis. Most of the studies were of a one-group pretest/posttest design that did not allow data extraction for comparisons between studies. Key findings from the review include:(Pellegrino, Krob, and Orkin 2021, e12454)
- Improved learning outcomes were reported in more studies that were without skill practice compared with studies that had skill practice. For clinical outcomes, more studies reported improved results with skill practice compared with studies without skill practice. However, it was noted that all clinical outcomes were self-reported and unverified.
- Training times varied from less than or equal to 15 minutes (brief) to 16 to 60 minutes for stand-alone programs and more than 60 minutes for opioid education embedded in other programs. There was not a consistent relationship identified between overdose education and naloxone distribution training duration and educational outcomes.
- In two studies enrolling 173 participants, no statistical difference was found between training versus no training among those lay persons who reported providing first aid interventions.
The scoping review concludes that results show that lay responders are engaged and able to learn to recognize opioid overdose, provide first aid and to summon advanced medical care appropriately (Pellegrino, Krob, and Orkin 2021, e12454).
Insights and Implications
Although there was no evidence that overdose education and naloxone distribution education improved the odds of receiving naloxone, this may simply reflect the ease of access to naloxone post-education. A significant number of knowledge gaps were identified in the scoping review that will require further research to strengthen first aid education guidelines.
Opioid Education and Naloxone Distribution
Last Full Review: American Red Cross Scientific Advisory Council Position 2020
A position statement was completed by the American Red Cross Scientific Advisory Council in 2020 on overdose education programs and naloxone distribution programs in the community (American Red Cross Scientific Advisory Council 2020a).
Red Cross Guidelines
- Overdose education programs and naloxone distribution programs should be widely available to the community.
- Overdose education programs should include training on naloxone administration, the potential complications of naloxone administration, and the management of these complications.
Evidence Summary
The age-adjusted rate of drug overdose deaths in the United States (U.S.) has increased over 17 years from 6.1 per 100,000 in 1999 to 21.7 per 100,000 in 2017, leading the U.S. Department of Health and Human Services to declare the opioid epidemic a public health emergency (CDC 2023; NSC 2018). Those with opioid addiction are also at risk for contracting infectious diseases, adding to the burden on society. Opioid education and naloxone distribution programs are associated with a reduced mortality from opioid overdose (Walley et al. 2013, f174; Naumann et al. 2019, 107536). Programs that distribute naloxone widely in communities and provide education show that the lay public can be taught to recognize opioid overdose and administer naloxone. This can lead to a measurable reduction of mortality in the population (Walley et al. 2013, f174; Naumann et al. 2019, 107536; Irvine et al. 2018, e218; Irvine et al. 2019, 1602; Wagner et al. 2010, 186).
Insights and Implications
Overdose is the leading cause of unintentional death in the United States, with opioids accounting for about two-thirds of those deaths. The Red Cross provides public educational programs that teach opioid overdose education, including the recognition of opioid overdose, use of the overdose reversal agent naloxone, and the importance of activating emergency services.
Self-Directed Digital Basic Life Support Training
Last Full Review: ILCOR 2021
The Red Cross has been a pioneer over the last decade in bringing quality resuscitation courses in digital format to the market. The courses offer learner-centered experiences and the use of visuals, including photos and videos. Self-directed, digital-based learning has been particularly popular among students during the coronavirus 2019 (COVID-19) pandemic to complete course work without the risk of disease transmission. To maintain a perspective on the value of self-directed digital education and training, it is important to compare them to instructor-led courses and training.
Red Cross Guidelines
- Basic life support course content and skills may be offered to adult and high-school aged children through:
- Instructor-led training, including manikin practice.
- Blended learning as:
- A self-directed online session to gain knowledge and understanding of the information and an in-person automated manikin practice session with feedback for skill training.
- A self-directed online session to gain knowledge and understanding of the information and an in-person, instructor-led session for skill practice with manikin practice and feedback.
Evidence Summary
A 2021 systematic review and Consensus on Science with Treatment Recommendations (CoSTR) (Wyckoff et al. 2022, e645; Bray et al. 2021) by the International Liaison Committee on Resuscitation (ILCOR) compared self-directed digital-based Basic Life Support (BLS) training for adults and children with traditional instructor-led training.
Patient-centered outcomes that were sought included good neurological outcome at hospital discharge or 30 days, survival at hospital discharge or 30 days, return of spontaneous circulation (ROSC), rates of bystander cardiopulmonary resuscitation (CPR), bystander CPR quality during out-of-hospital cardiac arrest and rates of automated external defibrillator (AED) use.
Educational outcomes that were sought at the end of training and within 12 months included CPR quality and AED competency, CPR and AED knowledge and confidence and willingness to perform CPR. Self-directed, digital-based BLS training included any form of digital education or training for BLS that can be completed without an instructor, except for mass media campaigns, such as videos with or without self-directed manikin practice, phone application-based, internet-based, game-based learning, virtual reality and augmented reality.
The reviewers included a total of 41 studies; overall certainty of evidence was very low to moderate across outcomes due primarily to risk of bias. A narrative synthesis of findings per outcome and by digital training medium (e.g., video or interactive computer programs with manikin practice) was reported. The reader is referred to the CoSTR for full details of this thorough, multifaceted review (Wyckoff et al. 2022, e645; Bray et al. 2021).
In summary, the ILCOR CoSTR (Bray et al. 2021) reported that:
- Comparable educational outcomes were shown for most CPR skills and knowledge gained immediately following training and up to 1 year with both instructor-led training and digital training using video or interactive computer programs with manikin practice.
- Comparable educational outcomes were shown for most CPR skills and knowledge gained immediately following training and up to 1 year, and overall CPR competency and knowledge immediately for both instructor-led training and digital training using video only.
- Instructor-led training for AED skills may be more effective immediately following training, but not in the long term.
- For most studies, there was no difference between instructor-led and digital-based instruction for outcomes of mean compression depth and proportion of compressions with correct depth, chest compression fraction, complete chest recoil, ventilation rate and hand position during compressions. For overall CPR skill competency judged by instructors, results were mixed, although more studies found no difference between instructor-led training and digital training.
- For AED competency, most studies reported instructor-led training to be superior; failures in the digital groups included failure to “clear during analysis and shock” or to activate the AED.
- For CPR knowledge, AED knowledge, confidence and willingness to perform CPR, most studies reported that there was no difference between instructor-led and digital training groups.
- For long-term CPR and AED knowledge and skills that were measured between 2 months and 12 months, the majority of studies reported no differences between groups for chest compression rates and depth.
- Use of videos with self-directed manikin practice was the most commonly used mode of instruction and was comparable to instructor-led training for most educational outcomes. Limited evidence for video-only training and outcomes of overall CPR competence and knowledge immediately after training favored instructor-led training or showed no difference between training modes (Bray et al. 2021).
The ILCOR CoSTR (Wyckoff et al. 2022, e645; Bray et al. 2021) led to strong treatment recommendations for the use of instructor-led training (with manikin practice with feedback device) or the use of self-directed training with video kits (instructional video and manikin practice with feedback device) for the acquisition of CPR theory and skills in lay adults and high-school aged (older than 10 years) children. In addition, a strong recommendation was made for instructor-led training (with AED scenario and practice) or the use of self-directed video kits (instructional video with AED scenario) for the acquisition of AED theory and skills in lay adults and high-school aged (older than 10 years) children. A weak recommendation was made suggesting the use of BLS video education (without manikin practice) when instructor-led training or self-directed training with video kits (instructional video plus manikin with feedback device) are not accessible, or when quantity over quality of BLS training is needed in adults and children.
Insights and Implications
Digital-based training for BLS gained popularity during the COVID-19 pandemic and demand for this mode of education remains strong. Although instructor-led training may be superior to digital training for some AED skills, the reviewers considered the significant improvement in AED skills attained with both methods compared with groups without training to be of greater importance because of voice prompts found on newer AEDs. Several important limitations of this review are acknowledged in the online CoSTR, such as variability in manikins used in the included studies and their technical specifications.
With its popularity among learners, digital training will likely be an active research topic going forward. In addition, the comparison of blended learning techniques that include instructor-led practice versus automated manikins requires further study.
Basic Life Support Training for High-Risk Populations
Last Full Review: ILCOR 2022
More than 356,000 out-of-hospital cardiac arrests occur annually in the United States, with most occurring at home or at a residence (73.9 percent) (Tsao et al. 2022). Layperson-initiated cardiopulmonary resuscitation (CPR) occurs in 40.8 percent of out-of-hospital cardiac arrests. Overall survival to hospital discharge for 2021 using Cardiac Arrest Registry to Enhance Survival (CARES) data was 9.1 percent, and with layperson CPR, 11.0 percent (Cardiac Arrest Registry to Enhance Survival 2021). For patients identified at high risk for out-of-hospital cardiac arrest, does the targeted training of family members or caregivers in basic life support (BLS) lead to improved patient or educational outcomes?
Red Cross Guidelines
- Family and caregivers of patients at high risk for out-of-hospital cardiac arrest should be trained in, or encouraged to be trained in, basic life support.
Evidence Summary
A 2022 systematic review and Consensus on Science with Treatment Recommendations (Wyckoff et al. 2022; Bray et al. 2022) by the International Liaison Committee on Resuscitation (ILCOR) focused on BLS training of likely rescuers, such as family members or caregivers, for adults and children at high risk of out-of-hospital cardiac arrest, compared with no training. This review was an update of a 2015 review (Finn et al. 2015, e203; Cartledge et al. 2016, 70) that examined the evidence for effectiveness of providing BLS training to family members of high-risk cardiac patients. New studies identified since the 2015 review included likely rescuers of patients with cardiac disease, drug use disorder, pulmonary disease or an acute life-threatening event. Meta-analysis of outcomes was not possible due to heterogeneity in BLS training methods, control groups and outcome assessment. Few studies evaluated patient outcomes from targeted BLS training for family members, and the limited number of witnessed out-of-hospital cardiac arrests and the loss to follow-up limited the certainty of the evidence identified (Wyckoff et al. 2022; Bray et al. 2022).
For studies that assessed educational outcomes, improvement in BLS skills and knowledge immediately after training were found in most studies. For long-term outcomes, although there was some degradation of some BLS skills, there was an improvement in skills and knowledge compared with baseline. Basic life support training was also found to increase willingness and confidence to provide CPR and to share training with other family members and friends (Wyckoff et al. 2022; Bray et al. 2022).
ILCOR recommends BLS training for likely rescuers of populations at high risk of out-of-hospital cardiac arrest. A good practice statement was made recommending that healthcare professionals encourage and direct likely rescuers of populations at high risk of cardiac arrest to attend BLS training (Wyckoff et al. 2022; Bray et al. 2022).
Insights and Implications
A large percentage of out-of-hospital cardiac arrests take place in the home or at a residence. This review confirms positive outcomes with BLS training, including competency in skills and improved confidence and willingness to provide CPR, and it supports guidelines recommending BLS training for family members or caregivers of patients at high risk for out-of-hospital cardiac arrest.
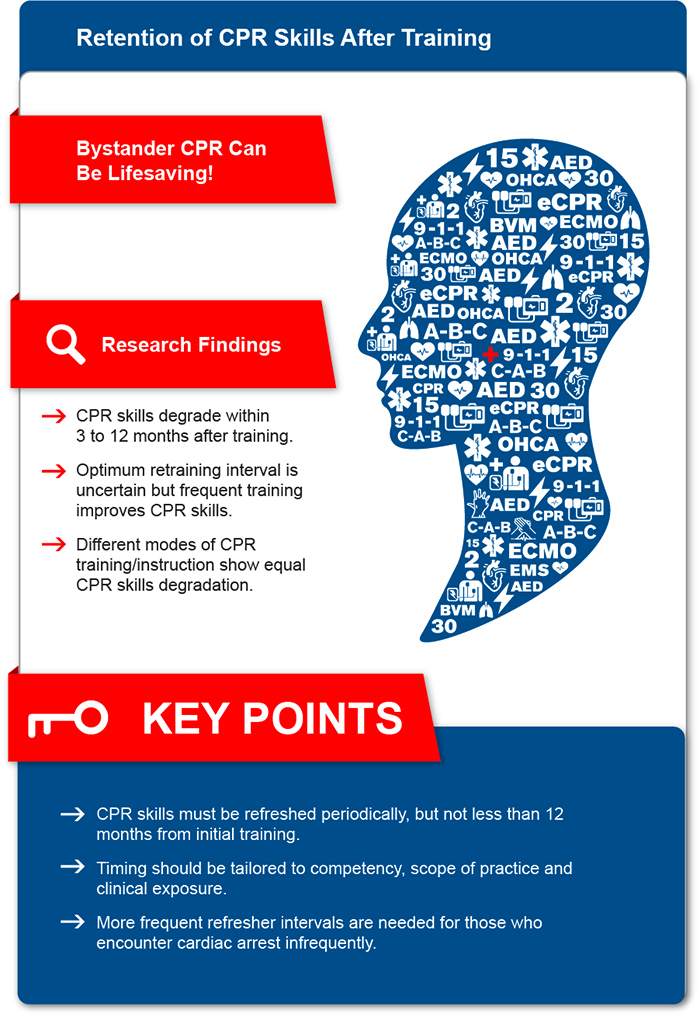
Retention of CPR Skills After Training
Last Full Review: American Red Cross Scientific Advisory Council 2009
Last Update: 2022
Bystander cardiopulmonary resuscitation (CPR) is associated with increased rates of survival following cardiac arrest. Past reviews have shown skill decay within 3 months of training and recommendations have been made for retraining at 1 to 2 years. Is there new evidence to suggest an ideal period for refreshing CPR skills after initial training?
Red Cross Guidelines
- Cardiopulmonary resuscitation (CPR) skills must be refreshed periodically but not less than 12 months from initial training.
- More frequent CPR refresher intervals are suggested for healthcare professionals with low frequency use of CPR skills. Interval timing should be tailored to competency, scope of practice and clinical exposure.
Evidence Summary
A 2022 triennial review (American Red Cross Scientific Advisory Council, 2022) of an American Red Cross Scientific Advisory Council scientific review aimed to look for evidence to determine how long after training or retraining in CPR is the ability retained to perform effective CPR. Studies of CPR skill retention that were identified are heterogeneous due to the many types of training, the multiple modes of teaching and the varying levels of trainees. Many forms of primary instruction were equally associated with CPR performance degradation and no form of primary instruction was shown to be superior in preventing degradation of skills. The authors of the review note that given the heterogeneity of the published research and the lack of standardized testing of skill retention, it is difficult to say with certainty what the optimal retraining schedule should be. However, more frequent refresher intervals are suggested and may be accomplished by establishing periodic personalized scheduling of performance training and assessment in the clinical environments, or through spaced learning with initial training.
Insights and Implications
There continues to be insufficient evidence to recommend the optimum interval or method for BLS retraining for laypersons. Because there is evidence of skills decay within 3 to 12 months after BLS training as well as evidence that frequent training improves CPR skills, the Red Cross suggests that individuals who encounter cardiac arrest less often consider more frequent training.
Spaced Learning Versus Massed Learning in Resuscitation Training
Last Full Review: ILCOR 2020
An International Liaison Committee on Resuscitation (ILCOR) systematic review (Yeung et al. 2020, 61) and Consensus on Science with Treatment Recommendations (Greif et al. 2020, S222) evaluated the use of “spaced learning” compared with “massed learning,” or training provided at one single time with all learners taking all resuscitation or first aid course types.
Red Cross Guidelines
- Course directors and planners may consider providing spaced learning (training or retraining distributed over time including blended formats and adaptive learning) instead of massed learning (training provided at one single time point) for resuscitation education.
Evidence Summary
In the ILCOR review (Greif et al. 2020, S222; Yeung et al. 2020, 61), spaced learning included the separation of training into several discrete sessions over a prolonged period with measurable intervals between training sessions, while a second type of spaced learning included the use of booster training, or distributed practice after the initial completion of training, such as for cardiopulmonary resuscitation (CPR). Booster training included just-in-time training, just-in-place training and refreshers. Seventeen randomized controlled trials (RCTs) and non-RCTs were included in a narrative synthesis involving Basic Life Support, Pediatric Advanced Life Support (PALS), and Neonatal Life Support courses using manikins and simulation. Certainty of evidence was very low for all outcomes and heterogeneity prohibited meta-analysis (Yeung et al. 2020, 61). The narrative review overall noted: (Berg et al. 2020, S92)
- Improved skill performance at 1 year after course completion for spaced learning in basic life support.
- A greater number of participants able to provide chest compressions of adequate depth at intervals up to 1 year with use of booster training.
- Improved CPR performance with spaced learning and monthly practice.
- Improved clinical performance scores among healthcare professionals in PALS with spaced learning compared with massed learning; decreased median time to start compressions following in-hospital cardiac arrest training sessions compared to standard course training.
- Improved neonatal intubation performance with booster training (once weekly or four consecutive days) compared with standard training.
No evidence was found reporting performance at clinical resuscitation, but one observational study reported an association with decreased mortality in newborns at 24 hours following booster training on delivery room management of the newborn (Mduma et al. 2015, 1).
A weak recommendation by ILCOR suggests that for learners taking resuscitation courses, spaced learning may be used instead of massed learning (Greif et al. 2020, S222).
Insights and Implications
Very low-certainty evidence supports the use of spaced learning in resuscitation education. It is likely that the benefit of spaced learning would be observed in other courses, such as First Aid or adult Advanced Life Support, although no studies were identified. There was some suggestion of difficulty maintaining ongoing motivation with spaced learning, and it may be challenging to engage students in repeated (spaced) learning. Spaced learning can be provided in methods that may gain the benefit and negate some of the challenges. Educators can use blended methods of online courses in single or multiple sittings combined with in-person sessions, based on student choice. Educators can also use blended with adaptive to provide spaced learning.
Blended Learning for Basic, Advanced and Trauma Life Support Education
Last Full Review: ILCOR 2022
Last Update: 2024
Blended learning uses self-directed online sessions to gain knowledge and understanding of information combined with an in-person, instructor-led skill session with manikin practice and feedback or with an automated manikin skill practice session with feedback for skills training. Self-directed, digital-based learning has been popular among students of Basic Life Support (BLS) courses during the coronavirus 2019 (COVID-19) pandemic and has been shown to result in comparable educational outcomes for most cardiopulmonary resuscitation (CPR) skills and knowledge when compared with traditional instructor-led training.
Red Cross Guidelines
- Basic life support course content and skills may be offered to adults and high school-aged children through:
- Instructor-led training, including manikin practice.
- Blended learning as:
- A self-directed online session to gain knowledge and understanding of the information and an in-person or virtual automated manikin skill practice session with feedback.
- A self-directed online session to gain knowledge and understanding of the information and an in-person, instructor-led session skill practice session with manikin practice and feedback.
- Blended learning may be considered for advanced life support education and training where resources and accessibility permit.
Evidence Summary
A 2022 International Liaison Committee on Resuscitation (ILCOR) systematic review (Elgohary et al. 2022, 100240) and Consensus on Science with Treatment Recommendations (CoSTR) (Wyckoff et al. 2022; Lockey et al. 2022) sought to compare a blended learning approach for participants taking an accredited life support course (e.g., BLS, Advanced Life Support [ALS], Pediatric Advanced Life Support, advanced trauma life support [ATLS]) with a non-blended learning approach (stratified to subgroups of online-only and face-to-face-only). Outcomes of interest included knowledge acquisition, skill acquisition, participant satisfaction, patient survival and implementation outcomes. A previous 2021 ILCOR CoSTR (Wyckoff et al. 2021, e645) led to a strong treatment recommendation for the use of instructor-led training (with manikin practice with feedback device) or the use of self-directed training with video kits, including manikin practice with feedback device, for the acquisition of CPR theory and skills in lay adults and high school age children.
Most of the studies identified in the current review used face-to-face-only training only as the control group. Results from BLS studies for outcomes of BLS knowledge and skills were reported as mixed, with some finding a benefit from blended learning and some finding no difference (Wyckoff et al. 2022; Lockey et al. 2022). A financial benefit was identified from a single study for teaching BLS with a blended learning approach (Castillo et al. 2019, 127).
For adult ALS, most studies reported no significant difference in knowledge and skills (post-course) between blended learning and non-blended learning approaches (Wyckoff et al. 2022; Lockey et al. 2022).
For ATLS, a single study (Dyer et al. 2021, e16811) was identified and reported that a blended learning approach that substituted elements of didactic material with online learning was better than an in-person-only approach for knowledge outcomes (Wyckoff et al. 2022; Lockey et al. 2022)
On the basis of the ILCOR CoSTR, a strong recommendation was made for a blended learning as opposed to a non-blended learning approach for life support training where resources and accessibility permit implementation (Wyckoff et al. 2022; Lockey et al. 2022).
Insights and Implications
This review found that a blended learning approach results in similar educational outcomes for participants as does a non-blended learning approach and may have a financial benefit. There was evidence of positive attitudes to all forms of training for BLS, while ALS course participants were divided over preference for blended learning versus face-to-face. Blended learning allows training on the participants’ own time and training in remote locations but requires resources including Internet or video access. Future studies are needed to determine if blended learning for life support education results in better patient outcomes. The Red Cross guidelines for use of blended learning with BLS courses remain unchanged, while a new guideline provides the option for ALS coursework, where feasible.
CPR Feedback Devices in Training
Last Full Review: ILCOR 2020
Last Update: 2024
An International Liaison Committee on Resuscitation (ILCOR) systematic review and Consensus on Science and Treatment Recommendations evaluated the use of a cardiopulmonary resuscitation (CPR) feedback device or guidance device for students receiving resuscitation training (Greif et al. 2020, S222). In addition, the American Red Cross Scientific Advisory Council has reviewed this topic and the ILCOR review is consistent with the findings of the American Red Cross Scientific Advisory Council.
Red Cross Guidelines
- Prompt/feedback devices should be used during training for cardiopulmonary resuscitation (CPR) to enable immediate feedback to students and improve the quality of CPR performance.
Evidence Summary
For laypersons trained with a CPR feedback device compared with no device, the ILCOR review identified one randomized controlled trial (RCT) (Zhou et al. 2020, 73) that reported no difference in CPR performance at 1 year post-training. A second RCT (Griffin et al. 2014, 264) with healthcare providers found that both the feedback group and the control group improved CPR performance at 1 year post-training, with no improvement difference between the groups. Improvements in retention of CPR skills with the use of feedback devices were reported at 7 days to 3 months post-training by four RCTs (Zhou et al. 2020, 73; Cortegiani et al. 2017, e0169591; Katipoglu et al. 2019; Smereka et al. 2019, e15995) for laypersons or healthcare professionals. For the outcome of CPR performance at the end of training, conflicting results from eight RCTs were reported on the use of feedback devices, with a trend towards improved CPR skills at the end of training (Greif et al. 2020, S222).
A weak recommendation by ILCOR suggests the use of feedback devices that provide directive feedback on compression rate, depth, release and hand position during CPR training (low-certainty evidence). It is suggested that if feedback devices are not available, to use tonal guidance (music or metronome) during training to improve compression rate only (low-certainty evidence) (Greif et al. 2020, S222).
Insights and Implications
The studies included generally showed positive short-term effects on retention of CPR skills with the use of feedback devices.
Hemorrhage Control Trainer Requirements
Last Full Review: American Red Cross Scientific Advisory Council 2020
Although hemorrhage control trainers are currently available to help educate learners, little is known about the ideal characteristics of an optimal hemorrhage control trainer. The 2020 American Red Cross Scientific Advisory Council review evaluated features of currently available hemorrhage control trainers to assess best practices.
Red Cross Guidelines
Low-fidelity hemorrhage control trainers should:
- Contain durable product that will withstand hundreds of uses.
- Not contain latex.
- Have average dimensions of an adult human arm.
- Be portable to allow for transport.
- Be priced in an affordable range that would allow for widespread distribution to resources that would benefit from training.
- Employ technologies that do not encumber the educational mission of the device.
High-fidelity hemorrhage control trainers should:
- Have material that has realistic tissue densities, does not contain latex and allows for decontamination.
- Have a circumference that allows for adequate tourniquet application.
- Allow for application of a tourniquet proximally and for direct manual pressure.
- Have anatomic landmarks, weight and other characteristics (such as articulating joints) to allow for a realistic simulation experience.
- Have a real-time feedback mechanism that demonstrates the need for continuous appropriate pressure.
- Have a real-time feedback mechanism that demonstrates appropriate application of a tourniquet.
- Have the ability to detect force from both direct pressure and a tourniquet.
- Be preprogramed to allow for varying scenario bleeding presentations.
- Provide a multisensory experience that simulates the presence of bleeding and barriers to application (such as voice prompts, presence of fluids).
Evidence Summary
An American Red Cross Scientific Advisory Council Answer was completed in 2020 to assess the best practices in design of hemorrhage control trainers. A literature search did not identify any reviews of best practices for hemorrhage control trainers. Several studies showed that tourniquet training and hemorrhage control training on a manikin allowed for subsequent successful application (Kragh et al. 2018, 36; Goolsby et al. 2019, 236; McCarty et al. 2019, 923). Hands-on training with the use of a hemorrhage control manikin has shown improved skills of wound packing and tourniquet application compared with didactic-only education (Zwislewski et al. 2019, 864). Cardiopulmonary resuscitation (CPR) feedback devices are recommended for training in CPR and are shown to improve the quality of CPR. Hemorrhage control manikin trainers are available with biofeedback on proper pressure application, with dimming of red lights to demonstrate enough pressure has been applied to stem the flow of blood and with a palpable femoral pulse. Other hemorrhage control trainer designs currently available on the market were described in this review.
Insights and Implications
Both the American Red Cross and the Stop the Bleed campaign advocate for the use of direct manual pressure, hemostatic dressings and tourniquets to treat life-threatening hemorrhage as appropriate (American Red Cross Scientific Advisory Council 2020c). Similar to other first aid and CPR training, practicing the psychomotor aspects of hemorrhage control can help in successful application of these methods and can help motivate the learner to act when faced with life-threatening bleeding. This review evaluates features of currently available hemorrhage control trainers and features available on CPR feedback trainers, and it suggested low- and high-fidelity features for design of a hemorrhage control trainer.
Team and Leadership Competency Training
Last Full Review: ILCOR 2020
Last Update: 2023
Team competencies in resuscitation are nontechnical skills and behaviors that include team-related communication, leadership, team dynamics and task allocation. These competencies are intended to improve overall team efficiency and patient outcomes. Specific leadership training in resuscitation courses was recommended by the International Liaison Committee on Resuscitation (ILCOR) in 2020 (Greif et al. 2020, S222; Kuzovlev et al. 2021,126). A 2024 ILCOR systematic review of team competencies adds to the evidence previously identified supporting leadership training (Farquharson et al. 2024, 100687).
Red Cross Guidelines
- It is reasonable to include team competencies in life support training.
Evidence Summary
A 2024 ILCOR systematic review (Farquharson et al. 2024, 100687) and Consensus on Science with Treatment Recommendations (CoSTR) (Farquharson et al. 2023; Greif et al. 2024) aimed to assess life support training with a specific emphasis on team competencies for learners, compared with life support training without emphasis on team competencies. Details and findings of the 17 studies included in the review can be found in the online CoSTR (Farquharson et al. 2023).
For the outcome of cardiopulmonary resuscitation (CPR) skills and quality at course completion, two randomized controlled trials (RCTs) reported shorter time to initiate at least one key skill (e.g., chest compressions). No effect was found on CPR performance from team competence training in eight RCTs and one observational study, and no difference was found at 4 months and 6 months after CPR training in two RCTs.
Various RCTs evaluating team competencies at course completion reported more leadership statements, increased team-directed communication, increased closed-loop communication and higher teamwork verbalizations (e.g., directed orders, tasks, planning).
Improved decision-making, leadership behavior, teamwork and workload management were reported in some RCTs (Farquharson et al. 2023; Greif et al. 2024). One RCT (Hunziker et al. 2010, 1086) reported that leadership instruction in volunteer medical students after a simulated CPR scenario resulted in more leadership statements, task assignments and commands, and decisions—with sustained efficacy at 4 months.
In the summary discussion, the CoSTR authors noted that several studies reported that team competencies training improved CPR skill performance, which persisted beyond course completion, and while study findings related to team competency training outcomes varied but were mostly positive. A weak suggestion was made by ILCOR based on very low-certainty evidence suggesting that teaching team competencies be included in basic life support and advanced life support training (Farquharson et al. 2023; Greif et al. 2024).
Insights and Implications
While the studies in this systematic review reported mixed results for the outcomes evaluated, the authors noted that previous clinical studies suggest that a lack of team competencies is a barrier to successful resuscitation, and team competencies have been associated with improved technical skill performance during clinical resuscitation attempts. The ideal instructional design or strategy for training of team competencies is unknown.
Cardiac Arrest Centers
Last Full Review: ILCOR 2020
Last Update: 2024
In 2015, the International Liaison Committee on Resuscitation (ILCOR) performed a review evaluating the transportation of adults and children in out-of-hospital cardiac arrest (OHCA) to a specialized cardiac arrest center (Bhanji et al. 2015, S242). The review included observational studies that evaluated clinical outcomes in OHCA patients transported to facilities with varying capabilities, including critical care, coronary angiography, hypothermic temperature control and post-resuscitation care. These studies reported an association between transport to a cardiac arrest center and survival-to-hospital discharge, but there was inconsistency in hospital factors related to optimal patient outcomes. The review concluded that specialized cardiac arrest centers may be effective despite a lack of high-quality data to support their implementation. The recommendation was made that OHCA patients be considered for transport to a specialized cardiac arrest center as part of a wider regional system of care for management of these patients.
Definitions of cardiac arrest centers have varied over the past decade—with some including hypothermic temperature control and neuroprognostication in a multimodal approach. However, the objective of cardiac arrest centers remains the same: to improve clinical outcomes through optimal management. An updated ILCOR systematic review of cardiac arrest centers in 2019 noted the lack of a widely accepted definition of a cardiac arrest center. The review included studies evaluating care of adults with attempted resuscitation after nontraumatic in-hospital cardiac arrest (IHCA) or OHCA at a cardiac arrest center, a regionalized cardiac arrest care center, a high case-volume center or similarly described facility, compared with care in a facility not designated as a specialized cardiac arrest center. The 2019 review found that compared with non-cardiac arrest centers, patients cared for at cardiac arrest centers had a greater likelihood of survival-to-hospital discharge and/or favorable neurological outcomes. However, care at cardiac arrest centers did not improve survival to 30 days or 30-day survival with favorable neurological outcome. In addition, for patients with ongoing cardiopulmonary resuscitation, care at cardiac arrest centers was not shown to improve return of spontaneous circulation (ROSC) after arrival compared with other non-cardiac arrest center hospitals.
Since the 2019 ILCOR review, additional studies evaluating cardiac arrest centers have been published, triggering an updated systematic review.
Red Cross Guidelines
- Patients in cardiac arrest should be transported by emergency medical services (EMS) to the most appropriate facility, based on local and regional EMS protocols.
Evidence Summary
A 2024 updated systematic review (Boulton et al. 2024, 110387) and Consensus on Science with Treatment Recommendations (Yeung et al. 2024; Greif et al. 2024) by ILCOR examined adults and children with attempted resuscitation after nontraumatic IHCA or OHCA who received care at a specialized cardiac arrest center, compared with care in an institute not designated as a specialized cardiac center.
Definitions
For this review, the definition of cardiac arrest centers by the Association for Acute Cardiovascular Care of the European Society of Cardiology considered the following (Sinning et al. 2020, S193):
- Specialized institutions offering all recommended treatment options for patients with OHCA, including:
- Access to a coronary angiography laboratory with 24/7 percutaneous coronary intervention (PCI) capability
- Targeted temperature management (TTM)
- Extracorporeal membrane oxygenation
- Mechanical ventilation
- Neurological prognostication
- Specialized Institutions with the capability for two or more of the preceding interventions and explicitly referred to by study authors as cardiac arrest centers, or synonymous terms such as:
- Critical care medical center
- Tertiary heart center
- Regional center
Studies that used high volume (as determined by the number of cases or patients) or PCI capability as the only distinguishing characteristic were excluded.
Of the 16 included studies, there was only one randomized controlled trial (RCT); the remaining were observational studies. Overall, the observational studies showed that care at a cardiac arrest center was associated with:
- Improved survival to 30 days with favorable neurological status
- Improved hospital discharge with favorable neurological status
- Improved survival to 30 days
- Improved survival to hospital discharge
- Improved ROSC
There was a high degree of heterogeneity, and meta-analysis was not possible. The one RCT that was included did not show a difference in any outcomes, but findings were limited to non-ST-elevation myocardial infarction patients with ROSC in a prehospital, urban setting. The evidence included was considered to be of very low certainty. An updated ILCOR treatment recommendation from this consensus on science suggests that adults with OHCA should be cared for in cardiac arrest centers.
Insights and Implications
In the United States, regionalized care has been developed for patients with trauma, acute stroke and ST-elevation myocardial infarction (STEMI)—with evidence for improved outcomes. Within these systems of care are different level designations that reflect the capabilities of a hospital to care for an acute event. Emergency medical services (EMS) protocols exist to help direct stroke, trauma and STEMI patients to the nearest appropriate level of care. Cardiac arrest centers are a next step for improving outcomes in patients with OHCA, but there will need to be a framework established like that for acute stroke or trauma, and coordination with EMS systems for emergency transportation.
Of the 15 observational studies included in the 2024 ILCOR updated systematic review, three were from the U.S. (Kragholm et al. 2017, e003414; Mumma et al. 2015, 516; Spaite et al. 2014, 496)—all reporting beneficial outcomes associated with transport to a PCI center (Kragholm et al. 2017, e003414) (PCI 24/7), a STEMI center (PCI 24/7 and TTM) (Mumma et al. 2015, 516) and a cardiac receiving center (coronary angiography/PCI, TTM and statewide regionalization) (Spaite et al. 2014, 496). Data were sourced from the registries of two studies, as well as one before-and-after study (i.e., a non-cardiac arrest center and a cardiac arrest center before and after state regionalization). Additional studies are needed to help identify which patients might benefit from designated cardiac arrest centers or specialty cardiac care centers. The Red Cross guidelines reflect the current processes for transporting OHCA patients.

